Wegovy (semaglutide 2.4 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. As more patients using Wegovy undergo surgical procedures, understanding how this medication interacts with anaesthesia has become essential for patient safety. Wegovy slows gastric emptying, which may increase aspiration risk during general anaesthesia. Current UK guidance from the Centre for Perioperative Care, Royal College of Anaesthetists, and Association of Anaesthetists generally supports continuing GLP-1 receptor agonists for most elective procedures, with individualised risk assessment. Patients must inform their surgical team and anaesthetist about Wegovy use to ensure appropriate perioperative planning and safety measures.
Quick Answer: Wegovy is generally continued for most elective surgeries in the UK, with individualised risk assessment by anaesthetists to manage potential aspiration risk from delayed gastric emptying.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. As surgical procedures become more common among patients using Wegovy, understanding the interaction between this medication and anaesthesia is essential for patient safety.
GLP-1 receptor agonists like Wegovy slow gastric emptying, which means food remains in the stomach for longer periods. This pharmacological effect raises considerations in the perioperative setting. Delayed gastric emptying may increase the risk of aspiration during general anaesthesia—a complication where stomach contents enter the lungs. The evidence for this risk is primarily based on case reports and observational data, with risk varying by individual factors.
Wegovy has a half-life of approximately one week, though the clinical effects on gastric emptying may persist for varying periods. Current UK anaesthetic guidance (from the Centre for Perioperative Care, Royal College of Anaesthetists, and Association of Anaesthetists) generally supports continuing GLP-1 receptor agonists for most elective procedures, with individualised risk assessment and mitigation strategies.
Patients scheduled for surgery should inform their surgical team and anaesthetist that they are taking Wegovy as early as possible. This allows adequate time for medication management planning and appropriate fasting protocols. Your anaesthetist may recommend additional precautions such as a liquid-only diet for 24 hours before surgery or use of gastric ultrasound assessment.
For emergency surgery, there may be insufficient time for detailed planning, so it's crucial to inform emergency medical staff about your Wegovy use to ensure appropriate anaesthetic management.
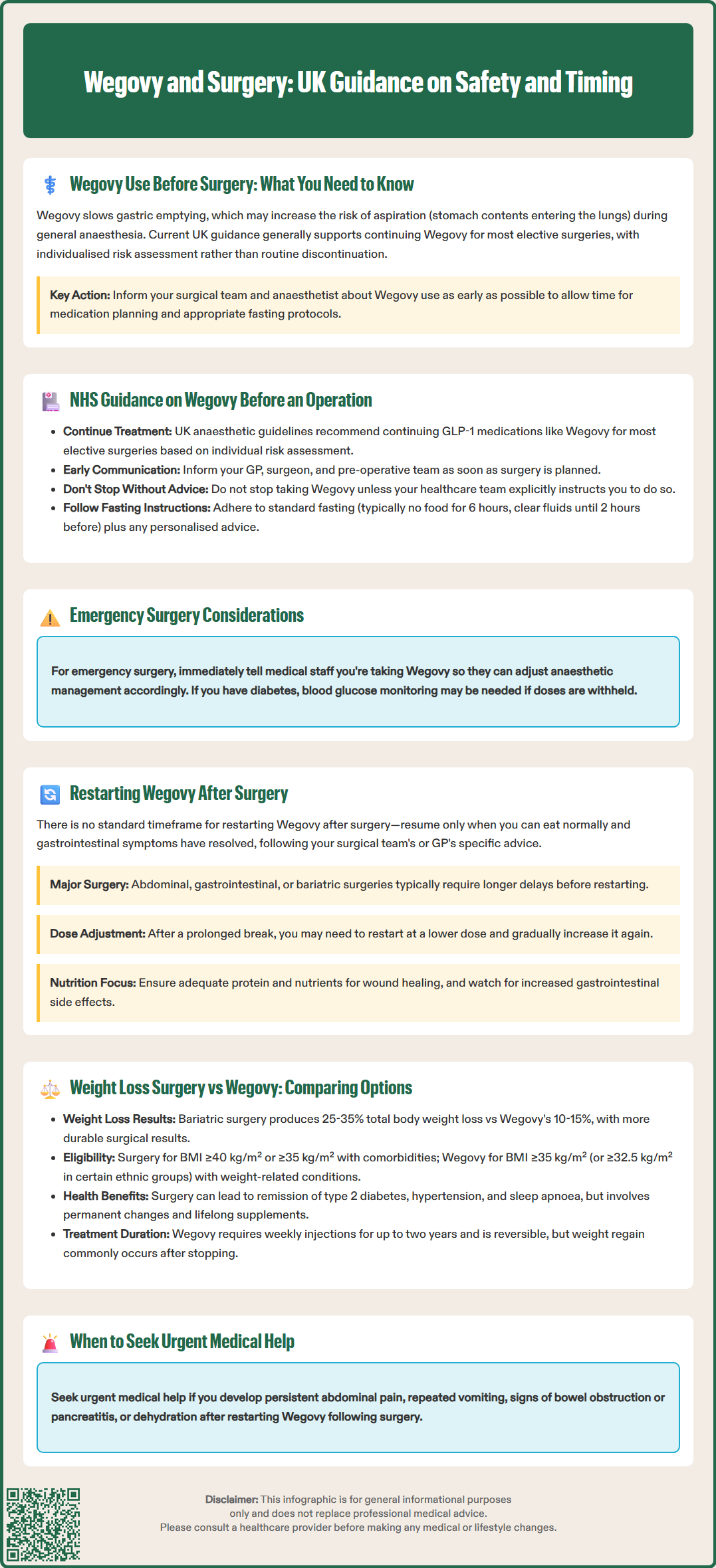
Current UK guidance from anaesthetic and surgical bodies generally supports continuing GLP-1 receptor agonists for most patients undergoing elective surgery. The Centre for Perioperative Care, Royal College of Anaesthetists and Association of Anaesthetists recommend an individualised approach based on risk assessment rather than routine discontinuation.
For elective (planned) surgery under general anaesthesia or deep sedation, your anaesthetist will assess your individual risk factors, including:
Current gastrointestinal symptoms (nausea, vomiting, abdominal pain)
Whether you are in the dose escalation phase of treatment
Other factors that might increase aspiration risk
The nature and urgency of your surgery
Key steps for patients include:
Inform your GP, surgeon, and pre-operative assessment team that you are taking Wegovy as soon as surgery is planned
Follow your anaesthetist's specific advice—this will be individualised based on your circumstances and local hospital protocols
Do not stop Wegovy without explicit instruction from your healthcare team
Maintain standard fasting instructions (typically nothing to eat for six hours and clear fluids up to two hours before surgery, though local policies may vary)
If you have diabetes and use Wegovy or another GLP-1 receptor agonist, additional monitoring of your blood glucose may be needed if any doses are withheld.
For emergency surgery, inform emergency medical staff immediately about your Wegovy use. Anaesthetists will implement appropriate safety measures based on your individual risk assessment.
NHS pre-operative assessment clinics now routinely ask about GLP-1 medications. If you have not been asked, volunteer this information proactively to ensure your surgical team can plan appropriately for your anaesthetic care.
Restarting Wegovy following surgery requires careful consideration of wound healing, post-operative recovery, and gastrointestinal function. There is no universal protocol, and decisions should be individualised based on the type of surgery performed, post-operative complications, and overall recovery progress.
There is no standardised UK timeframe for restarting Wegovy after surgery. The general principle is to resume treatment only when oral intake is adequate and any gastrointestinal symptoms have resolved. Always follow the specific advice from your surgical team or GP before restarting treatment.
Following major abdominal surgery, gastrointestinal procedures, or operations with complications, a longer delay is usually necessary. Wegovy's effects on gastric motility and appetite suppression could potentially interfere with adequate nutritional intake during the critical healing phase. For bariatric surgery or bowel operations, reintroduction should be under specialist review within your multidisciplinary team.
Important considerations when restarting Wegovy:
After a prolonged interruption, you may need to restart at a lower dose and re-titrate gradually, as advised in the Wegovy product information
Monitor for increased gastrointestinal side effects, which may be more pronounced post-operatively
Ensure adequate protein and nutrient intake to support wound healing
Seek urgent medical advice for persistent or worsening abdominal pain, repeated vomiting, signs of bowel obstruction or pancreatitis, or dehydration
Patients should have a clear plan documented at hospital discharge regarding when and how to restart Wegovy. If this information is not provided, contact your GP or the hospital team for clarification before resuming treatment. Never restart Wegovy without medical guidance following surgery.
If you experience side effects from Wegovy, report them to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Both bariatric surgery and Wegovy represent evidence-based interventions for significant weight loss, but they differ substantially in mechanism, efficacy, risks, and suitability for different patient populations. Understanding these differences helps patients and clinicians make informed decisions aligned with individual circumstances and preferences.
Bariatric surgery (including gastric bypass, sleeve gastrectomy, and gastric banding) produces substantial, sustained weight loss—typically 25-35% of total body weight—and can lead to remission of type 2 diabetes, hypertension, and obstructive sleep apnoea. NICE recommends considering bariatric surgery for adults with a BMI of 40 kg/m² or more, or 35-40 kg/m² with significant obesity-related comorbidities, when non-surgical measures have been unsuccessful. NICE also recommends considering surgery for people with a BMI of 30-34.9 kg/m² who have recent-onset type 2 diabetes. Lower BMI thresholds may apply for people from certain ethnic backgrounds. According to the National Bariatric Surgery Registry, surgery carries procedural risks, requires lifelong dietary modifications and nutritional supplementation, and involves permanent anatomical changes.
Wegovy, by contrast, is a non-invasive pharmacological option producing average weight loss of 10-15% of body weight in clinical trials. NICE guidance (TA875) supports its use in adults with BMI ≥35 kg/m² (or ≥32.5 kg/m² in certain ethnic groups) with at least one weight-related comorbidity, as part of a specialist weight management service. Treatment is typically provided for up to two years. Wegovy requires ongoing weekly injections, and weight regain commonly occurs if treatment is discontinued.
Key comparison points:
Magnitude of weight loss: Surgery typically produces greater absolute weight loss than Wegovy
Durability: Surgical weight loss tends to be more durable; Wegovy requires continued treatment
Risks: Surgery carries immediate procedural risks; Wegovy has a different side effect profile (predominantly gastrointestinal)
Reversibility: Wegovy can be stopped; most bariatric procedures are permanent or difficult to reverse
Cost and access: Both require specialist referral through NHS weight management services; availability varies by region
Some patients may benefit from Wegovy as part of preparation for surgery, under specialist guidance. Others may find Wegovy sufficient to meet their health goals without surgery. Increasingly, evidence suggests these approaches may be complementary rather than competing—some patients benefit from pharmacotherapy following bariatric surgery to optimise long-term weight maintenance. Decisions should be made collaboratively with specialist weight management teams, considering individual medical history, preferences, and treatment goals.
Current UK guidance generally supports continuing Wegovy for most elective procedures, with your anaesthetist making an individualised decision based on your specific risk factors. Always inform your surgical team about Wegovy use as early as possible to allow appropriate planning.
Restart Wegovy only when oral intake is adequate and gastrointestinal symptoms have resolved, following specific advice from your surgical team or GP. After major abdominal or gastrointestinal surgery, a longer delay is usually necessary, and you may need to restart at a lower dose.
Wegovy slows gastric emptying, meaning food remains in the stomach longer, which may increase the risk of aspiration (stomach contents entering the lungs) during general anaesthesia. Your anaesthetist will assess your individual risk and implement appropriate safety measures.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.