
Wegovy (semaglutide 2.4 mg) is a GLP-1 receptor agonist licensed for weight management in adults with obesity or overweight with comorbidities. Whilst highly effective, NICE guidance emphasises that Wegovy must be prescribed alongside a reduced-calorie diet and increased physical activity. A well-structured Wegovy meal plan is essential to optimise weight loss, preserve lean muscle mass, prevent nutrient deficiencies, and manage common gastrointestinal side effects. This article provides evidence-based guidance on building balanced, nutritious meal plans that work synergistically with Wegovy to support sustainable weight management and overall health throughout treatment.
Quick Answer: A Wegovy meal plan should provide adequate protein (1.2–1.5 g/kg ideal body weight), complex carbohydrates, healthy fats, and fibre within a calorie-controlled diet, whilst managing gastrointestinal side effects through smaller, frequent meals and strategic food choices.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for weight management in adults with obesity or overweight with weight-related comorbidities. The medication works by mimicking the natural hormone GLP-1, which regulates appetite and food intake by acting on areas of the brain that control hunger. Wegovy temporarily slows gastric emptying, increases feelings of fullness after eating, and reduces appetite, making it easier to consume fewer calories.
Whilst Wegovy is highly effective at promoting weight loss—clinical trials demonstrate average weight reductions of 10–15% of body weight over 68 weeks—it is not a standalone solution. NICE guidance (TA875) emphasises that semaglutide should be prescribed alongside a reduced-calorie diet and increased physical activity as part of a comprehensive weight management programme. In the NHS, Wegovy is typically available through specialist weight management services for people with a BMI ≥35 kg/m² with weight-related comorbidities (with lower thresholds for some populations), and treatment is limited to a maximum of 2 years.
Importantly, Wegovy must not be used during pregnancy or breastfeeding. Women of childbearing potential should use effective contraception and discontinue Wegovy at least 2 months before a planned pregnancy. People with diabetes taking insulin or sulfonylureas may need dose adjustments to prevent hypoglycaemia when starting Wegovy.
Nutrition plays a crucial role in optimising outcomes with Wegovy. A well-planned meal approach ensures adequate intake of essential nutrients whilst working synergistically with the medication's appetite-suppressing effects. Without proper nutritional planning, patients may experience nutrient deficiencies, excessive muscle loss, or difficulty sustaining weight loss long-term. Understanding how to structure meals appropriately helps maximise the benefits of Wegovy whilst minimising potential adverse effects and supporting overall health during the weight loss journey.
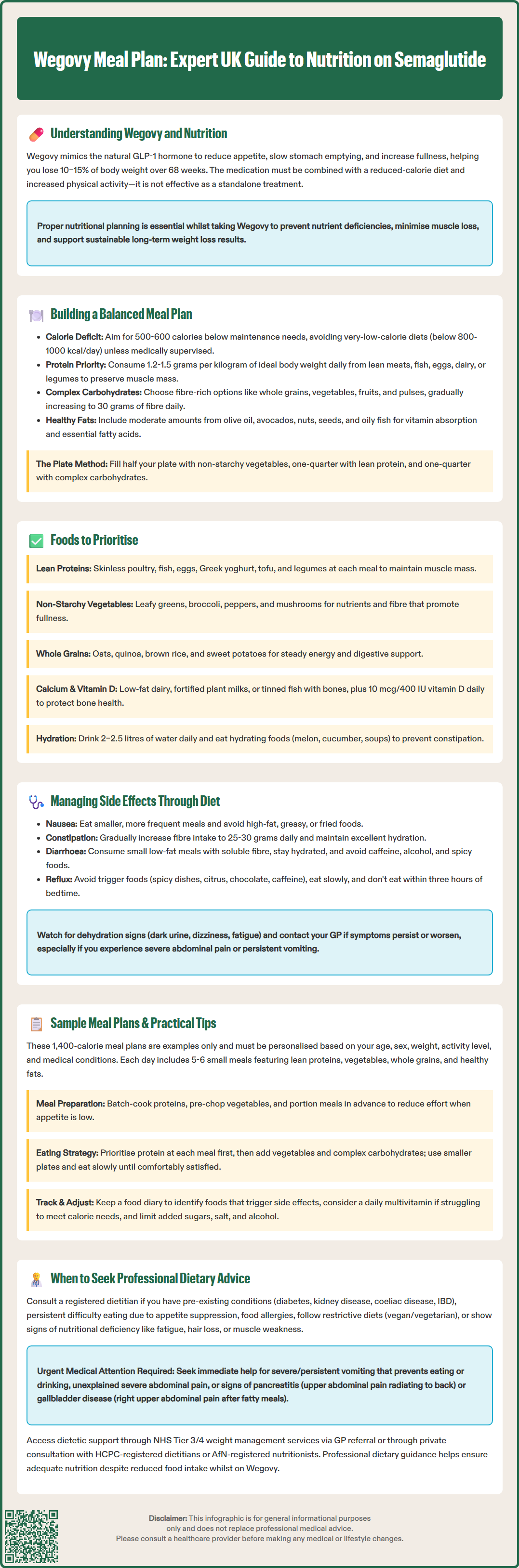
Creating a balanced meal plan whilst taking Wegovy requires careful attention to nutritional adequacy despite reduced appetite and smaller portion sizes. The foundation should be a calorie-controlled diet that creates a sustainable deficit—typically 500–600 kcal below maintenance requirements—whilst ensuring sufficient intake of macronutrients and micronutrients. Energy needs are highly individual and depend on age, sex, weight, activity level and medical conditions; the NHS Eatwell Guide provides general principles, but personalised advice from a healthcare professional may be beneficial.
Protein intake is particularly important during weight loss to preserve lean muscle mass. Aim for 1.2–1.5 grams of protein per kilogram of ideal body weight daily, distributed across meals, though this should be adjusted for certain medical conditions (consult your healthcare provider if you have kidney disease, liver disease or are elderly/frail). High-quality protein sources include lean meats, fish, eggs, dairy products, legumes, and plant-based alternatives. Adequate protein also helps maintain satiety and supports the body's metabolic functions during caloric restriction.
Carbohydrates should focus on complex, fibre-rich sources such as whole grains, vegetables, fruits, and pulses. These provide sustained energy, essential vitamins and minerals, and dietary fibre that supports digestive health—particularly important given Wegovy's gastrointestinal side effects. Gradually increase fibre intake to reach the recommended 30 grams daily from varied sources, as sudden increases may worsen digestive symptoms.
Healthy fats remain essential despite calorie reduction. Include moderate amounts of unsaturated fats from sources like olive oil, avocados, nuts, seeds, and oily fish. These support absorption of fat-soluble vitamins (A, D, E, K) and provide essential fatty acids. Portion control is key, as fats are calorie-dense.
Structure meals around the 'plate method': half the plate with non-starchy vegetables, one-quarter with lean protein, and one-quarter with complex carbohydrates. This visual approach simplifies portion control and ensures balanced nutrition across the day.
Very-low-calorie diets (below 800–1000 kcal/day) should be avoided unless specifically prescribed and medically supervised.
Certain foods are particularly beneficial when taking Wegovy, supporting both weight loss goals and overall nutritional health. Lean protein sources should form the cornerstone of each meal: skinless poultry, white fish, shellfish, eggs, low-fat Greek yoghurt, cottage cheese, tofu, and legumes. These foods provide essential amino acids with relatively few calories, helping maintain muscle mass during weight reduction.
Non-starchy vegetables deserve generous inclusion in your meal plan as tolerated. Leafy greens, broccoli, cauliflower, peppers, courgettes, mushrooms, tomatoes, and cucumber are nutrient-dense, low in calories, and high in fibre. They add volume to meals, promoting fullness whilst delivering vitamins, minerals, and antioxidants essential for health. Increase portions gradually to minimise digestive discomfort.
Whole grains and complex carbohydrates provide sustained energy without causing rapid blood glucose spikes. Prioritise oats, quinoa, brown rice, wholemeal bread, sweet potatoes, and barley. These foods contain B vitamins, iron, and fibre that support digestive function—particularly valuable given Wegovy's effects on gastric motility.
Calcium-rich foods warrant special attention, as reduced food intake may compromise bone health. Include low-fat dairy products, fortified plant-based alternatives, tinned fish with bones (sardines, salmon), and leafy greens. Adequate calcium intake, combined with vitamin D (from oily fish, fortified foods, or a 10 microgram/400 IU daily supplement during autumn/winter or year-round if limited sun exposure), supports skeletal health during weight loss.
Hydrating foods and fluids are crucial. Water should be the primary beverage, with a target of 2–2.5 litres daily (discuss with your healthcare provider if you have heart or kidney disease). Herbal teas, fruit juice limited to 150 ml per day, and water-rich foods like melon, cucumber, and soups contribute to hydration status, which is particularly important for managing constipation—a common Wegovy side effect.
If following a vegan or vegetarian diet, pay particular attention to vitamin B12, iodine, calcium and protein sources; consultation with a registered dietitian may be beneficial.
Wegovy commonly causes gastrointestinal side effects, particularly during dose escalation. Strategic dietary choices can significantly reduce the severity and frequency of these symptoms. Nausea, the most frequently reported adverse effect, can be managed through several approaches:
Eat smaller, more frequent meals rather than three large meals. This reduces gastric distension and works with Wegovy's delayed gastric emptying.
Avoid high-fat, greasy, or fried foods, which slow digestion further and may exacerbate nausea.
Choose bland, easily digestible options when nausea occurs: plain crackers, toast, rice, bananas, and clear broths.
Consider separating food and fluid intake—drinking between meals rather than with meals may help prevent excessive fullness for some people.
Constipation affects many Wegovy users due to slowed gastrointestinal transit. Dietary management includes:
Gradually increase fibre intake to 25–30 grams daily from fruits, vegetables, whole grains, and pulses. Sudden increases may worsen symptoms, so build up slowly.
Maintain excellent hydration—inadequate fluid intake with high fibre can paradoxically worsen constipation.
Include natural laxative foods such as prunes, kiwi fruit, flaxseeds, and psyllium husk.
Regular physical activity supports bowel motility alongside dietary measures.
Diarrhoea may also occur. Management strategies include:
Eat small, low-fat meals throughout the day
Try soluble fibre (oats, psyllium) as tolerated to add bulk to stools
Stay hydrated with water and consider oral rehydration solutions if diarrhoea is persistent
Avoid caffeine, alcohol and spicy foods which may worsen symptoms
Reflux and indigestion may occur due to delayed gastric emptying. Avoid trigger foods (spicy dishes, citrus, tomatoes, chocolate, caffeine), eat slowly, remain upright after meals, and avoid eating within three hours of bedtime.
Be alert to signs of dehydration (dark urine, dizziness, fatigue) which can lead to acute kidney injury, especially in those with existing kidney disease or older adults. If gastrointestinal symptoms persist despite dietary modifications, or if you experience severe abdominal pain, persistent vomiting, or signs of dehydration, contact your GP or prescribing clinician promptly, or seek urgent care via NHS 111 or A&E if symptoms are severe. Consider consulting a pharmacist about suitable over-the-counter remedies.
If you experience any suspected side effects, report them to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
The following sample meal plans provide approximately 1,400 kcal per day. Please note that energy requirements vary significantly based on age, sex, weight, activity level and medical conditions. These are examples only and should be tailored to your individual needs—consult a healthcare professional for personalised advice.
Sample Day 1:
Breakfast: Porridge made with 40g oats, 200ml semi-skimmed milk, topped with 80g berries and 1 tablespoon ground flaxseed.
Mid-morning: 150g low-fat Greek yoghurt with a small handful of almonds (20g).
Lunch: Large mixed salad with 100g grilled chicken breast, cherry tomatoes, cucumber, peppers, and 1 tablespoon olive oil dressing. One small wholemeal roll.
Afternoon: Apple slices with 1 tablespoon peanut butter.
Dinner: 120g baked salmon fillet, 150g roasted sweet potato, steamed broccoli and green beans with lemon juice.
Evening: Small bowl of vegetable soup.
Sample Day 2:
Breakfast: Two-egg omelette with spinach, mushrooms, and tomatoes. One slice wholemeal toast.
Mid-morning: Pear and 30g reduced-fat cheese.
Lunch: Lentil and vegetable soup with a wholemeal pitta bread. Side salad.
Afternoon: Carrot and cucumber sticks with 2 tablespoons hummus.
Dinner: 100g lean beef mince Bolognese with courgette noodles ('courgetti') and 2 tablespoons grated Parmesan.
Evening: 80g berries with a small pot of low-fat fromage frais.
Practical implementation tips:
Meal preparation is invaluable—batch-cook proteins, chop vegetables, and portion meals in advance to reduce decision fatigue when appetite is low.
Use smaller plates and bowls to make appropriate portions appear more substantial.
Eat mindfully—chew thoroughly, eat slowly, and stop when comfortably satisfied rather than full.
Keep a food diary to identify patterns between specific foods and side effects.
Plan protein intake first at each meal, then add vegetables and complex carbohydrates.
Consider a daily multivitamin to safeguard against potential micronutrient gaps, particularly if struggling to meet calorie targets. Avoid vitamin A supplements if pregnant and check with your healthcare provider if you take warfarin or have kidney disease.
Limit added sugars, salt, and alcohol in line with NHS Eatwell guidance and the Chief Medical Officers' Low Risk Drinking Guidelines.
Whilst general dietary guidance supports most Wegovy users, certain circumstances warrant consultation with a HCPC-registered dietitian (find one via the British Dietetic Association) or AfN-registered nutritionist (listed on the UK Voluntary Register of Nutritionists). Referral should be considered if:
You have pre-existing medical conditions requiring specialised dietary management, such as diabetes, chronic kidney disease, coeliac disease, or inflammatory bowel disease. These conditions necessitate tailored nutritional approaches that balance disease management with weight loss goals.
You experience persistent difficulty meeting nutritional needs due to severe appetite suppression or ongoing gastrointestinal symptoms. A dietitian can develop strategies to ensure adequate nutrient intake despite reduced food volume.
You have food allergies or intolerances that significantly limit food choices, making balanced meal planning more complex.
You follow a restrictive dietary pattern (vegan, vegetarian) and need guidance ensuring adequate protein and micronutrient intake during caloric restriction.
You develop signs of nutritional deficiency: unusual fatigue, hair loss, brittle nails, muscle weakness, or frequent infections may indicate inadequate nutrient intake.
People with diabetes should monitor blood glucose levels closely when starting or titrating Wegovy and seek medication review, particularly if taking insulin or sulfonylureas, to prevent hypoglycaemia.
NHS Tier 3/4 specialist weight management services often include dietetic support as part of comprehensive programmes in line with NICE guidance (TA875). Your GP can refer you to local services, or you may access private dietetic consultation.
Contact your GP or prescribing clinician urgently if you experience severe or persistent vomiting preventing adequate nutrition or hydration, unexplained severe abdominal pain, signs of pancreatitis (severe upper abdominal pain radiating to the back), or symptoms of gallbladder disease (right upper abdominal pain, particularly after fatty meals). For severe or worsening symptoms, use NHS 111 or attend A&E as appropriate. Professional dietary guidance optimises your Wegovy treatment outcomes whilst safeguarding nutritional health throughout your weight loss journey.
Focus on lean proteins (chicken, fish, eggs, legumes), non-starchy vegetables, whole grains, and healthy fats within a calorie-controlled diet. Aim for 1.2–1.5 grams of protein per kilogram of ideal body weight daily, distributed across smaller, frequent meals to manage appetite suppression and side effects.
For nausea, eat smaller frequent meals, avoid high-fat and greasy foods, and choose bland options like toast and rice. For constipation, gradually increase fibre intake to 25–30 grams daily, maintain excellent hydration (2–2.5 litres water), and include natural laxative foods such as prunes and kiwi fruit.
A daily multivitamin may help safeguard against micronutrient gaps when food intake is reduced. Ensure adequate calcium and vitamin D (10 micrograms/400 IU daily supplement recommended during autumn/winter or year-round if limited sun exposure) to support bone health during weight loss.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.