What is a microdose of GLP-1? This term refers to using GLP-1 receptor agonist medications at doses substantially lower than those licensed by UK regulatory authorities such as the MHRA and NICE. Whilst standard therapeutic doses of semaglutide or liraglutide are carefully calibrated through extensive clinical trials, microdosing involves using a fraction of these established doses—often below licensed starting doses. This approach has emerged largely through social media, with individuals attempting to minimise side effects whilst seeking some therapeutic benefit. However, microdosing is not a licensed or evidence-based approach to GLP-1 therapy. Any deviation from licensed dosing regimens should only occur under close medical supervision, as the risk-benefit profile at sub-therapeutic doses remains poorly characterised.
Quick Answer: A microdose of GLP-1 is an informal term for using GLP-1 receptor agonist medications at doses substantially lower than those licensed by UK regulatory authorities, an approach that is not evidence-based or recommended.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereA microdose of GLP-1 (glucagon-like peptide-1) is an informal, non-standard term referring to the administration of GLP-1 receptor agonist medications at doses substantially lower than those licensed and recommended by UK regulatory authorities such as the MHRA (Medicines and Healthcare products Regulatory Agency) and NICE (National Institute for Health and Care Excellence). Whilst standard therapeutic doses of medications like semaglutide or liraglutide are carefully calibrated based on extensive clinical trials, microdosing typically involves using a fraction of these established doses—often below the licensed starting doses.
GLP-1 receptor agonists are a class of medications primarily licensed for the treatment of type 2 diabetes mellitus and, in some formulations, for weight management in adults with obesity or overweight with weight-related comorbidities. These medications work by mimicking the action of naturally occurring GLP-1, an incretin hormone produced in the intestine that regulates blood glucose levels and appetite. The concept of microdosing has emerged largely through social media and online communities, where individuals discuss using lower doses in an attempt to minimise side effects whilst potentially achieving some therapeutic benefit.
It is crucial to understand that microdosing is not a licensed or evidence-based approach to GLP-1 therapy. The doses approved by regulatory bodies have been determined through rigorous phase III clinical trials involving thousands of participants, with careful assessment of both efficacy and safety profiles. Prescribing outside the licensed indications and doses constitutes off-label use, which requires prescribers to document their rationale, obtain informed consent, and provide appropriate monitoring. Any deviation from licensed dosing regimens should only occur under close medical supervision, as the risk-benefit profile at sub-therapeutic doses remains poorly characterised and may not provide the intended clinical outcomes.
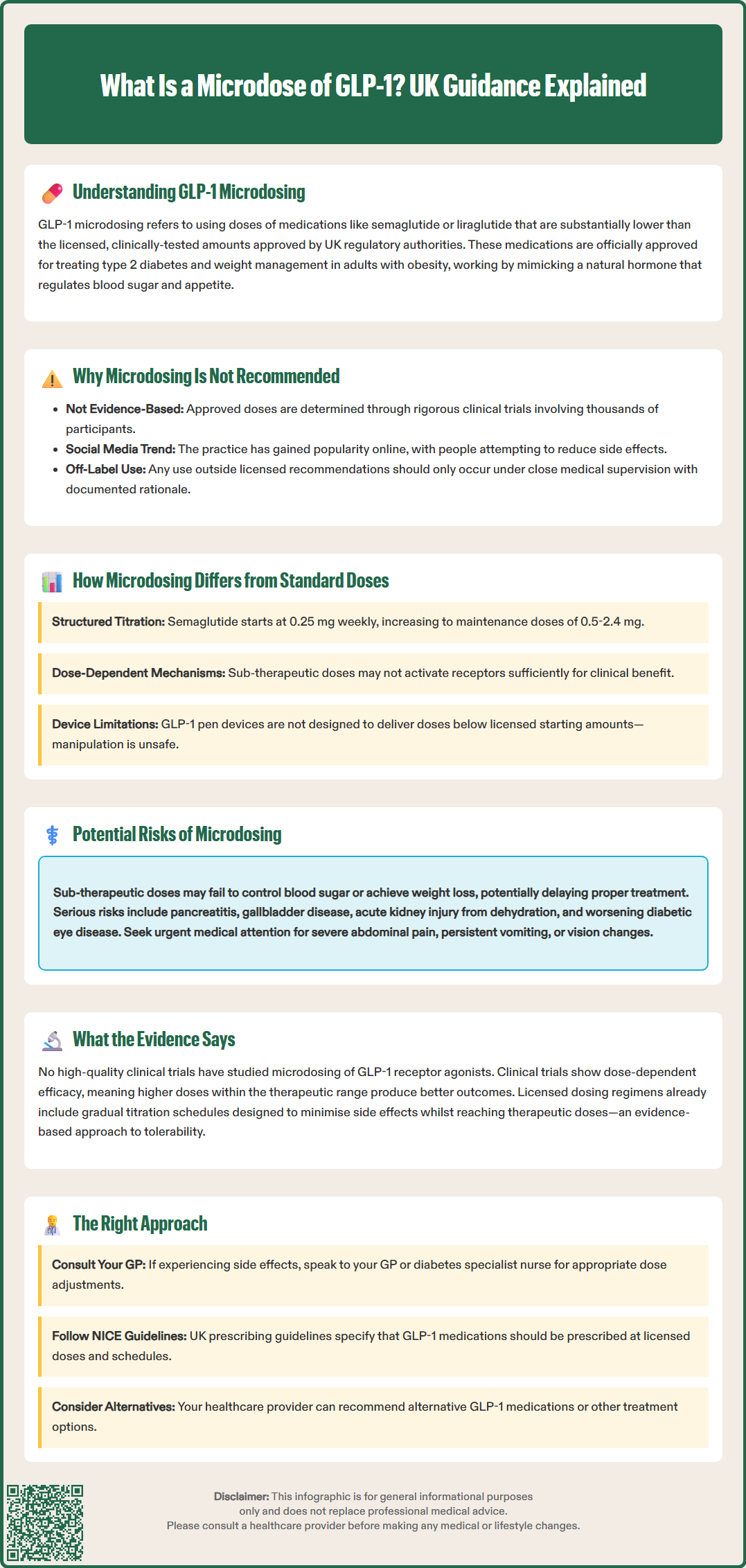
Standard dosing protocols for GLP-1 receptor agonists follow a carefully structured titration schedule designed to optimise therapeutic efficacy whilst allowing the body to adapt to the medication. For example, semaglutide for type 2 diabetes (Ozempic) typically begins at 0.25 mg weekly, gradually increasing to maintenance doses of 0.5 mg, 1 mg, or 2 mg. For weight management, semaglutide (Wegovy) follows a different schedule: 0.25 mg, 0.5 mg, 1.0 mg, 1.7 mg, and finally 2.4 mg weekly. Similarly, liraglutide for diabetes (Victoza) starts at 0.6 mg daily, escalating to 1.2 mg and potentially 1.8 mg if needed, while liraglutide for weight management (Saxenda) follows a schedule from 0.6 mg to 3.0 mg daily (via 1.2 mg, 1.8 mg, and 2.4 mg steps). These titration schedules are evidence-based and designed to minimise gastrointestinal adverse effects—the most common side effects of this drug class.
Microdosing, by contrast, involves maintaining doses below these established starting points or progressing more slowly than recommended. Some individuals may attempt to use doses lower than the licensed starting doses or remain at the initial dose indefinitely, rather than following the licensed escalation protocol. It is important to note that GLP-1 pen devices are not designed to deliver doses below their licensed starting doses, and attempting to manipulate devices to deliver micro-increments is unsafe and risks dosing errors.
This approach fundamentally differs from standard practice in several important ways:
Pharmacological effect: GLP-1 receptor agonists demonstrate dose-dependent effects on glycaemic control and weight reduction. Lower doses may not achieve the receptor activation required for meaningful clinical benefit.
Metabolic impact: The mechanisms by which these medications improve insulin secretion, suppress glucagon, delay gastric emptying, and reduce appetite are all dose-related. Sub-therapeutic doses may provide insufficient pharmacological activity.
Safety profile: Whilst lower doses might theoretically reduce the incidence of dose-dependent adverse effects such as nausea and vomiting, this has not been systematically studied, and the overall risk-benefit ratio remains unknown.
The standard dosing regimens have been established through extensive pharmacokinetic and pharmacodynamic studies, ensuring that therapeutic drug levels are achieved and maintained. Deviating from these protocols means operating outside the evidence base that supports the medication's use. In the UK, Wegovy (semaglutide 2.4 mg) is commissioned within specialist weight management services according to NICE criteria, not for general off-label use.
Proponents of GLP-1 microdosing often cite the potential for reduced side effects as the primary rationale for this approach. Gastrointestinal symptoms—particularly nausea, vomiting, diarrhoea, and constipation—are the most frequently reported adverse effects of GLP-1 receptor agonists, occurring in 20–50% of patients depending on the specific agent and dose according to clinical trials and SmPC data. The hypothesis underlying microdosing is that lower doses might provide some metabolic benefit whilst minimising these troublesome symptoms, potentially improving treatment adherence.
Some individuals also report using microdoses for appetite modulation without seeking the substantial weight loss associated with higher doses, or as a gentler introduction to the medication before escalating to standard doses. However, these purported benefits remain anecdotal and lack robust clinical evidence. There is no official link between microdosing and improved tolerability profiles, as this dosing strategy has not been subjected to controlled clinical trials.
The risks of microdosing are significant and multifaceted:
Therapeutic inefficacy: Sub-therapeutic doses may fail to achieve meaningful improvements in glycaemic control or weight management, potentially delaying appropriate treatment and allowing disease progression.
Unpredictable pharmacology: The dose-response relationship for both efficacy and safety has not been characterised at very low doses, creating uncertainty about what effects—beneficial or harmful—might occur.
Medication wastage and cost: Using medications outside their licensed indications may not be covered by NHS prescribing, leading to out-of-pocket expenses for patients. Current UK supply constraints make appropriate use of these medications particularly important.
Lack of monitoring: Individuals self-adjusting doses may not receive appropriate clinical monitoring for adverse effects or treatment response.
False reassurance: Patients may believe they are receiving treatment for their condition when, in reality, the dose is insufficient to provide clinical benefit.
Safety concerns: Important risks associated with GLP-1 receptor agonists include pancreatitis, gallbladder disease, dehydration leading to acute kidney injury, hypoglycaemia (when used with insulin or sulfonylureas), and potential worsening of diabetic retinopathy with rapid glycaemic improvement.
Patients should seek urgent medical attention if they experience severe persistent abdominal pain (which may indicate pancreatitis), persistent vomiting/dehydration, jaundice, acute visual changes, or hypoglycaemia if on insulin or sulfonylureas.
Women of childbearing potential should use effective contraception while taking GLP-1 receptor agonists. Semaglutide should be discontinued at least 2 months before a planned pregnancy due to its long half-life.
Patients considering any modification to their prescribed medication regimen should consult their GP or specialist before making changes. Self-directed dose adjustments can compromise treatment outcomes and patient safety. Suspected side effects should be reported to the MHRA via the Yellow Card scheme (yellowcard.mhra.gov.uk).
The current evidence base for GLP-1 receptor agonist therapy is derived from extensive clinical trial programmes that have established the efficacy and safety of specific, licensed doses. No high-quality clinical trials have specifically investigated microdosing as a therapeutic strategy. The doses studied in pivotal trials represent the minimum effective doses required to demonstrate statistically significant and clinically meaningful outcomes in glycaemic control, weight reduction, and cardiovascular risk reduction.
For instance, the SUSTAIN trial programme for semaglutide in type 2 diabetes demonstrated HbA1c reductions of 1.0–1.8% and weight loss of 3.5–6.5 kg at doses of 0.5–1.0 mg weekly. The STEP trials for semaglutide 2.4 mg in weight management showed mean weight loss of 14.9% from baseline at 68 weeks. The LEADER trial for liraglutide 1.8 mg demonstrated cardiovascular benefits in high-risk populations with type 2 diabetes. There is no evidence that doses below these levels provide comparable benefits.
Some pharmacokinetic studies have examined the lower end of the dose-response curve, but these were conducted to establish appropriate starting doses for titration, not to validate microdosing as a standalone strategy. The current evidence suggests that:
Dose-dependent efficacy: Both glycaemic and weight outcomes improve with increasing doses within the therapeutic range, suggesting that very low doses are unlikely to provide substantial benefit.
Tolerability: The gradual titration schedules incorporated into licensed regimens already represent an evidence-based approach to minimising adverse effects whilst achieving therapeutic doses.
Individual variation: Some patients may respond to lower doses due to individual pharmacokinetic or pharmacodynamic differences, but this should be assessed through proper clinical monitoring, not self-experimentation.
NICE guidance for the use of GLP-1 receptor agonists in type 2 diabetes (NG28) and for weight management (the current NICE Technology Appraisal for semaglutide 2.4 mg) specifies the use of licensed doses and titration schedules. Patients should be prescribed these medications according to their licensed indications and dosing regimens.
If standard doses are not tolerated, clinically appropriate alternatives might include slower titration (still within SmPC guidelines), switching to a different GLP-1 receptor agonist, considering other medication classes, enhancing diet/lifestyle support, or specialist review. UK prescribing should follow SmPC and NICE guidance; off-label microdosing is generally unsupported within NHS practice.
Anyone experiencing persistent side effects or concerns about their medication should contact their GP or diabetes specialist nurse for advice on appropriate dose adjustments or alternative treatments rather than self-adjusting their medication.
GLP-1 microdosing has not been studied in clinical trials, so its safety and efficacy remain unknown. Sub-therapeutic doses may fail to provide meaningful clinical benefit for diabetes or weight management and should only be considered under close medical supervision.
Semaglutide for diabetes (Ozempic) starts at 0.25 mg weekly, whilst semaglutide for weight management (Wegovy) begins at the same dose before titrating to 2.4 mg. Liraglutide for diabetes (Victoza) starts at 0.6 mg daily, and liraglutide for weight management (Saxenda) escalates from 0.6 mg to 3.0 mg daily.
No, you should not self-adjust your GLP-1 medication dose. If you experience persistent side effects such as nausea or vomiting, contact your GP or diabetes specialist nurse for advice on appropriate dose adjustments, slower titration, or alternative treatments.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.