Energy metabolism refers to the biochemical processes by which the body converts nutrients into usable energy, primarily stored as adenosine triphosphate (ATP). This fundamental system powers every cellular function, from muscle contraction and nerve transmission to maintaining body temperature. The body derives energy from three macronutrients—carbohydrates, fats, and proteins—each following distinct metabolic pathways. These processes occur continuously in every cell, with particularly high activity in the brain, heart, liver, and skeletal muscle. Understanding energy metabolism is essential for comprehending how the body maintains homeostasis, responds to nutritional intake, and adapts to varying energy demands. Disruptions can manifest as fatigue, weight changes, or serious metabolic disorders requiring clinical assessment.
Quick Answer: Energy metabolism is the series of biochemical processes that convert nutrients from food into adenosine triphosphate (ATP), the usable energy form that powers all cellular functions.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereEnergy metabolism refers to the complex series of biochemical processes by which the human body converts nutrients from food into usable energy. This energy, stored primarily as adenosine triphosphate (ATP), powers every cellular function—from muscle contraction and nerve transmission to protein synthesis and maintaining body temperature. Without efficient energy metabolism, cells cannot perform their essential roles, and bodily functions begin to deteriorate.
The body derives energy from three main macronutrients: carbohydrates, fats, and proteins. Each undergoes distinct metabolic pathways, but all ultimately contribute to ATP production. Carbohydrates are typically the body's preferred energy source, broken down into glucose for immediate use or stored as glycogen. Fats provide a concentrated energy reserve, particularly important during prolonged activity or fasting. Proteins have structural and functional roles in the body; they may be used for energy when other sources are depleted.
Energy metabolism occurs continuously in every cell, with particularly high activity in metabolically active tissues such as the brain, heart, liver, and skeletal muscle. The brain preferentially uses glucose but can utilise ketone bodies during prolonged fasting. The efficiency of these processes directly influences physical performance, cognitive function, and overall health. Understanding energy metabolism is fundamental to comprehending how the body maintains homeostasis, responds to nutritional intake, and adapts to varying energy demands throughout the day.
Disruptions to normal energy metabolism can manifest in various ways, from fatigue and weight changes to serious metabolic disorders. Healthcare professionals assess metabolic function through clinical examination, biochemical testing, and evaluation of symptoms to identify potential abnormalities requiring intervention.
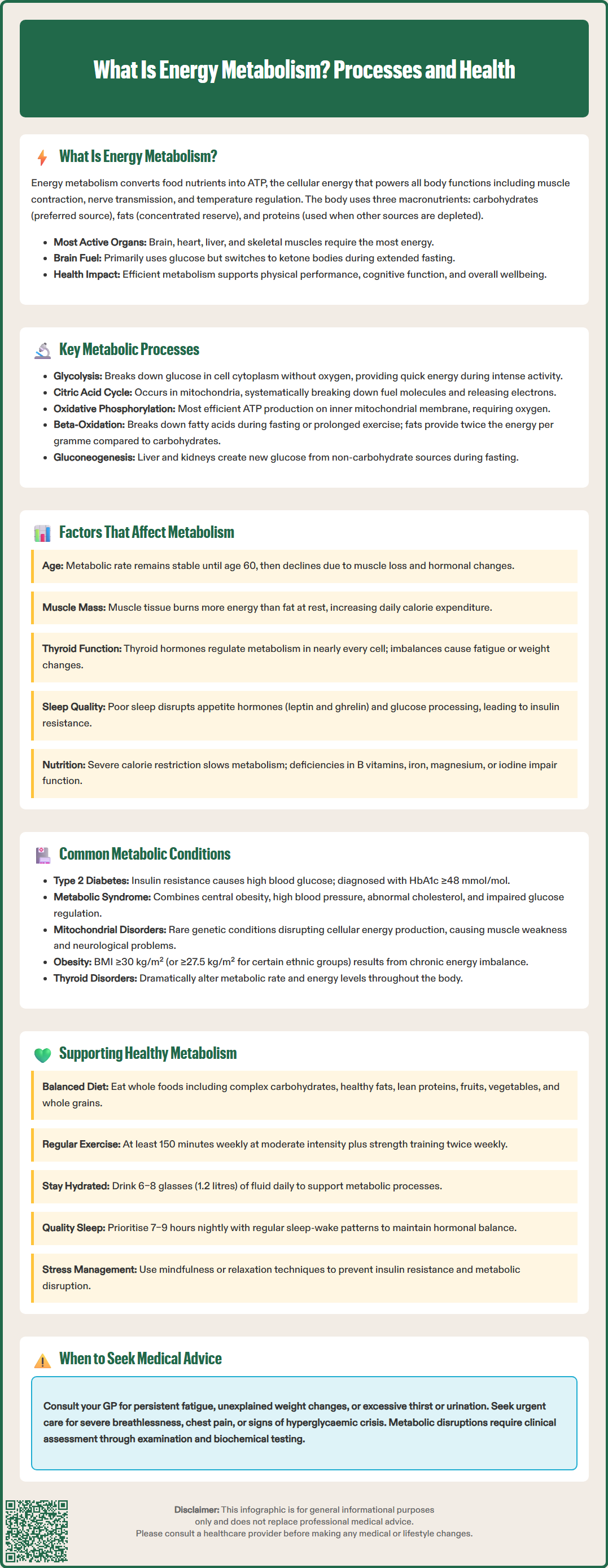
Energy metabolism encompasses several interconnected biochemical pathways, each with specific roles in extracting and storing energy. Glycolysis represents the initial breakdown of glucose in the cell cytoplasm, producing small amounts of ATP and pyruvate molecules. This anaerobic process (not requiring oxygen) provides rapid energy during intense activity but yields relatively little ATP compared to subsequent aerobic pathways. During anaerobic conditions, pyruvate is reduced to lactate, which can later be recycled back to glucose in the liver via the Cori cycle.
The citric acid cycle (also called the Krebs cycle or tricarboxylic acid cycle) occurs within mitochondria, the cell's powerhouses. Here, pyruvate and other fuel molecules are systematically broken down, releasing electrons that feed into the electron transport chain. This cycle is central to aerobic metabolism and generates carbon dioxide as a waste product, which is expelled through respiration.
Oxidative phosphorylation represents the most efficient ATP-generating process, occurring along the inner mitochondrial membrane. The electron transport chain creates a proton gradient that drives ATP synthase, producing the majority of cellular ATP. This process requires oxygen, explaining why adequate oxygenation is essential for sustained energy production.
Beta-oxidation describes the breakdown of fatty acids into acetyl-CoA units, which then enter the citric acid cycle. This pathway is particularly important during fasting, prolonged exercise, or low-carbohydrate states. Fats yield more than twice the energy per gram compared to carbohydrates, making them an efficient long-term energy store.
Additionally, gluconeogenesis allows the liver and kidneys to synthesise new glucose from non-carbohydrate sources (amino acids, lactate, glycerol) during fasting or carbohydrate restriction. These processes work in concert, regulated by hormones such as insulin, glucagon, cortisol, and thyroid hormones, to maintain stable blood glucose levels and ensure continuous energy availability to vital organs.
Numerous physiological and lifestyle factors influence the efficiency and rate of energy metabolism. Age impacts metabolic rate, with evidence suggesting relative stability until around age 60, followed by a more pronounced decline. This change is largely attributed to loss of lean muscle mass and hormonal changes. Children and adolescents generally exhibit higher metabolic rates to support growth and development.
Body composition plays a crucial role, as muscle tissue is metabolically more active than adipose (fat) tissue. Individuals with greater muscle mass typically have higher resting energy expenditure. Conversely, excess adipose tissue, particularly visceral fat, can contribute to metabolic dysfunction and insulin resistance.
Thyroid function is fundamental to metabolic regulation. Thyroid hormones (T3 and T4) directly influence the metabolic rate of nearly every cell. Hypothyroidism slows metabolism, causing fatigue, weight gain, and cold intolerance, whilst hyperthyroidism accelerates it, leading to weight loss, heat intolerance, and increased heart rate. Standard thyroid function tests typically include thyroid stimulating hormone (TSH) and, when indicated, free T4, with free T3 reserved for specific clinical scenarios such as suspected thyrotoxicosis, in line with NICE guidance.
Physical activity substantially affects energy expenditure, both during exercise and afterwards through elevated post-exercise oxygen consumption. Regular physical activity also improves mitochondrial function and insulin sensitivity, enhancing overall metabolic efficiency.
Nutritional status directly impacts metabolic processes. Severe caloric restriction can trigger adaptive thermogenesis, where the body reduces metabolic rate to conserve energy. Micronutrient deficiencies—particularly B vitamins, iron, magnesium, and iodine—can impair metabolic enzyme function. Sleep quality and duration also influence metabolism through effects on hormones regulating appetite (leptin and ghrelin) and glucose metabolism. Chronic sleep deprivation is associated with insulin resistance and altered energy balance. Genetic factors, medications (including beta-blockers, corticosteroids, and certain antipsychotics), and environmental temperature further modulate individual metabolic rates. Importantly, patients should never stop or change prescribed medications without consulting their healthcare provider.
Several medical conditions arise from or significantly affect energy metabolism. Type 2 diabetes mellitus represents a major metabolic disorder characterised by insulin resistance and impaired glucose metabolism. The body's cells become less responsive to insulin, leading to elevated blood glucose levels and disrupted energy utilisation. Diagnosis typically requires an HbA1c ≥48 mmol/mol (6.5%), though HbA1c may be unsuitable in certain situations including pregnancy, haemoglobinopathies, anaemia, or rapid-onset diabetes. Management focuses on lifestyle modification, blood glucose-lowering medicines, and potentially insulin therapy, as outlined in NICE guidance.
Metabolic syndrome encompasses a cluster of conditions—central obesity, hypertension, dyslipidaemia, and impaired glucose regulation—that collectively increase cardiovascular disease risk. This syndrome reflects widespread metabolic dysfunction affecting multiple organ systems and requires comprehensive management addressing each component.
Mitochondrial disorders represent a heterogeneous group of genetic conditions affecting cellular energy production. These rare but serious conditions can present with muscle weakness, neurological symptoms, cardiac dysfunction, and multi-organ involvement. Diagnosis often requires specialist investigation including muscle biopsy, genetic testing, and metabolic studies.
Thyroid disorders, as previously mentioned, profoundly affect metabolic rate. Both hypothyroidism and hyperthyroidism require appropriate investigation and treatment, typically managed in primary care with specialist input when necessary. The NHS provides comprehensive thyroid function testing and monitoring services.
Obesity itself represents a metabolic condition where energy intake chronically exceeds expenditure, leading to excessive fat accumulation. In the UK, obesity is generally defined as a BMI ≥30 kg/m² (or ≥27.5 kg/m² for some ethnic groups including South Asian, Chinese, Black African and African-Caribbean populations). This creates a pro-inflammatory state that further impairs metabolic function, creating a self-perpetuating cycle. NICE recommends a tiered approach to obesity management, from lifestyle interventions to pharmacotherapy and, in selected cases, bariatric surgery.
Other relevant conditions include chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME), where patients experience profound, unexplained fatigue. While the mechanisms remain incompletely understood, management focuses on supportive care and symptom control as outlined in NICE guidance. Inborn errors of metabolism—rare genetic disorders affecting specific metabolic pathways—require specialist metabolic physician input and often lifelong dietary management.
Maintaining optimal energy metabolism requires a multifaceted approach encompassing nutrition, physical activity, and lifestyle factors. Balanced nutrition forms the foundation, with emphasis on whole foods providing complex carbohydrates, healthy fats, lean proteins, and essential micronutrients. The NHS Eatwell Guide recommends a varied diet rich in fruits, vegetables, whole grains, and adequate protein whilst limiting processed foods, added sugars, and saturated fats.
Regular physical activity enhances metabolic health through multiple mechanisms. The UK Chief Medical Officers' Physical Activity Guidelines recommend at least 150 minutes of moderate-intensity aerobic activity weekly, combined with strength training exercises twice weekly. Both aerobic exercise and resistance training improve insulin sensitivity, increase muscle mass, and enhance mitochondrial function. Even modest increases in daily activity—such as walking, taking stairs, or active commuting—contribute meaningfully to metabolic health.
Adequate hydration supports metabolic processes, as water is essential for numerous biochemical reactions. Dehydration can impair physical and cognitive performance. The NHS recommends approximately 6–8 glasses (1.2 litres) of fluid daily, adjusted for activity level and climate. This can include water, lower-fat milk and sugar-free drinks, including tea and coffee.
Sleep hygiene deserves attention, as consistent, quality sleep (7–9 hours for most adults) supports hormonal balance and metabolic regulation. Establishing regular sleep-wake patterns and creating a conducive sleep environment can improve metabolic outcomes.
Stress management is increasingly recognised as important for metabolic health. Chronic stress elevates cortisol, which can promote insulin resistance and central fat deposition. Techniques such as mindfulness, relaxation exercises, and appropriate work-life balance may benefit metabolic function.
When to seek medical advice: Individuals experiencing unexplained persistent fatigue, unintentional weight changes, excessive thirst or urination, or other concerning symptoms should consult their GP. Urgent medical attention is needed for symptoms of hyperglycaemic crisis (marked thirst with frequent urination, dehydration, nausea/vomiting, abdominal pain, drowsiness/confusion, or rapid breathing), chest pain, severe breathlessness, or suspected acute adrenal insufficiency. Healthcare professionals can arrange appropriate blood tests (glucose, HbA1c, thyroid function, lipid profile) and provide evidence-based guidance tailored to individual circumstances. Early identification and management of metabolic dysfunction can prevent progression to more serious conditions and improve long-term health outcomes.
The main pathways include glycolysis (glucose breakdown in the cytoplasm), the citric acid cycle (occurring in mitochondria), oxidative phosphorylation (the most efficient ATP-generating process along the inner mitochondrial membrane), and beta-oxidation (fatty acid breakdown). These interconnected processes work together to extract energy from carbohydrates, fats, and proteins.
Thyroid hormones (T3 and T4) directly influence the metabolic rate of nearly every cell in the body. Hypothyroidism slows metabolism, causing fatigue, weight gain, and cold intolerance, whilst hyperthyroidism accelerates it, leading to weight loss, heat intolerance, and increased heart rate.
Consult your GP if you experience unexplained persistent fatigue, unintentional weight changes, excessive thirst or urination, or other concerning symptoms. Seek urgent medical attention for symptoms of hyperglycaemic crisis (marked thirst, frequent urination, confusion, rapid breathing), chest pain, severe breathlessness, or suspected acute adrenal insufficiency.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.