
Weight loss injections such as semaglutide and liraglutide have become increasingly prescribed for obesity management in the UK. Whilst these glucagon-like peptide-1 (GLP-1) receptor agonists effectively promote weight reduction through appetite suppression and metabolic changes, concerns about muscle loss during treatment are valid. Research indicates that approximately 20–30% of weight lost may comprise lean tissue, including muscle, rather than fat alone. However, this muscle loss results from the caloric deficit these medications facilitate, not from direct pharmacological muscle breakdown. Understanding how to preserve muscle mass through adequate protein intake, resistance training, and appropriate monitoring is essential for optimising treatment outcomes and maintaining functional capacity during weight loss.
Quick Answer: Weight loss injections do not directly cause muscle breakdown, but approximately 20–30% of weight lost may comprise lean tissue due to the caloric deficit these medications create.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide and liraglutide, work through several interconnected mechanisms to promote weight reduction. These medications mimic naturally occurring hormones in the gastrointestinal tract that regulate appetite and glucose metabolism.
Primary mechanisms of action include:
Appetite suppression – GLP-1 receptor agonists act on receptors in the hypothalamus, the brain's appetite control centre, reducing hunger signals and increasing feelings of satiety after meals
Delayed gastric emptying – These medications slow the rate at which food leaves the stomach, prolonging the sensation of fullness and reducing overall caloric intake (though this effect tends to attenuate with chronic use)
Glucose-dependent insulin secretion – By enhancing pancreatic beta-cell function, these injections increase insulin release only when blood glucose is elevated
Reduced glucagon secretion – Suppression of this hormone helps prevent excessive glucose production by the liver
The MHRA has approved several GLP-1 receptor agonists for weight management in adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² with weight-related comorbidities. However, NICE guidance (TA875 for semaglutide, TA664 for liraglutide) sets narrower NHS eligibility criteria, requiring treatment within specialist weight management services and specific BMI thresholds.
Weight loss results vary by medication: semaglutide 2.4mg (Wegovy) typically produces 10–15% weight reduction over 68 weeks, while liraglutide 3mg (Saxenda) generally achieves 5–8% at 56 weeks. According to SmPC guidance, treatment should be discontinued if less than 5% weight loss is achieved after 12 weeks on the maintenance dose.
The resulting caloric deficit from reduced food intake leads to weight loss, raising important questions about body composition changes, particularly regarding the preservation of lean muscle mass alongside fat loss.
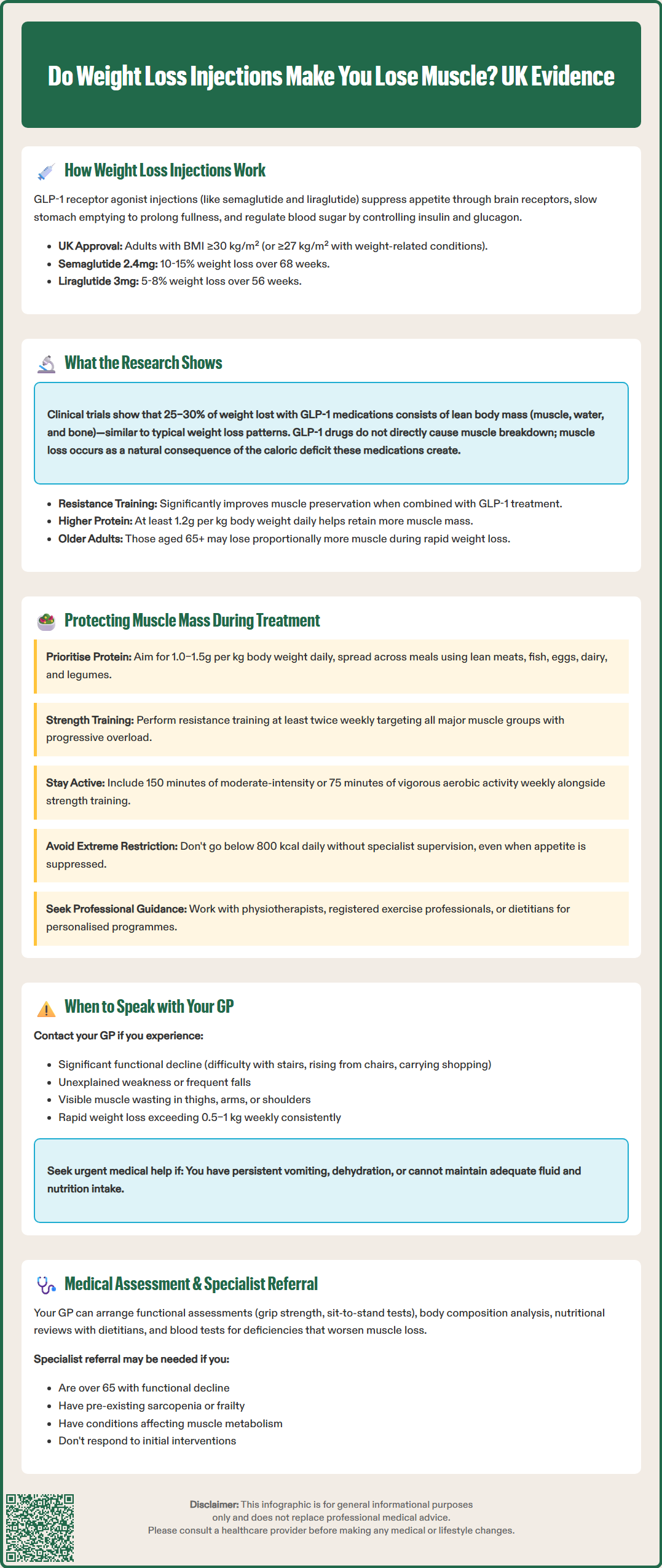
Maintaining muscle mass during weight loss treatment with injectable medications requires a proactive, multifaceted approach. Research indicates that without appropriate interventions, approximately 20–30% of weight lost during rapid reduction can come from lean tissue, including muscle, rather than fat alone.
Protein intake optimisation is fundamental to muscle preservation. Current evidence suggests adults using weight loss injections should aim for 1.0–1.5 grams of protein per kilogram of adjusted body weight daily, distributed across meals. High-quality protein sources include lean meats, fish, eggs, dairy products, legumes, and plant-based alternatives. This elevated protein intake provides essential amino acids necessary for muscle protein synthesis, even during caloric restriction. Patients with chronic kidney disease or other conditions affecting protein metabolism should seek guidance from their healthcare team before increasing protein intake.
Resistance training represents the most effective strategy for preserving muscle mass during weight loss. UK Chief Medical Officers' Physical Activity Guidelines recommend:
Strength training exercises at least twice weekly, targeting all major muscle groups
Progressive overload – gradually increasing resistance or repetitions to stimulate muscle adaptation
Compound movements such as squats, lunges, and press exercises that engage multiple muscle groups simultaneously
Aerobic activity – 150 minutes of moderate-intensity or 75 minutes of vigorous activity weekly
Patients should ideally work with qualified healthcare professionals, particularly when initiating resistance training programmes. Physiotherapists or CIMSPA-registered exercise professionals can design individualised programmes accounting for current fitness levels, mobility limitations, and any musculoskeletal conditions.
Adequate caloric intake remains crucial. Whilst GLP-1 receptor agonists suppress appetite, very low-calorie diets (<800 kcal daily) should only be followed under specialist supervision. Low-energy diets (800–1,200 kcal) require monitoring and nutritional adequacy assessment. Registered dietitians can help patients balance sufficient nutrition with the appetite-suppressing effects of these medications, ensuring nutritional adequacy whilst achieving weight loss goals.
Clinical trial data examining body composition changes during GLP-1 receptor agonist treatment provides important insights into muscle mass preservation. The STEP (Semaglutide Treatment Effect in People with obesity) trials, which informed regulatory approvals, demonstrated that whilst these medications produce substantial weight loss, body composition changes warrant careful consideration.
The STEP 1 trial published in the New England Journal of Medicine (2021) found that participants receiving semaglutide 2.4 mg weekly lost an average of 14.9% of their initial body weight over 68 weeks compared with 2.4% in the placebo group. A subsequent body composition substudy using dual-energy X-ray absorptiometry (DEXA) scans revealed that approximately 25–30% of this weight loss comprised lean body mass, which includes muscle tissue, water, and bone. This proportion aligns with typical weight loss patterns but highlights the importance of muscle-preserving strategies.
Key research findings include:
Studies combining GLP-1 receptor agonists with structured resistance training programmes show significantly better lean mass preservation compared to medication alone
Research indicates that higher protein intake (≥1.2 g/kg daily) during GLP-1 treatment correlates with improved muscle mass retention
Older adults (aged 65+) may experience proportionally greater muscle loss during rapid weight reduction, necessitating enhanced monitoring as per EWGSOP2 sarcopenia guidelines
It is important to note that there is no official link suggesting GLP-1 receptor agonists directly cause muscle breakdown through pharmacological mechanisms. Rather, muscle loss occurs as a consequence of the caloric deficit these medications facilitate. The muscle loss observed is not unique to injectable weight loss treatments but represents a general phenomenon during significant weight reduction from any cause.
Ongoing research continues examining long-term body composition outcomes and optimal strategies for preserving functional muscle mass during treatment.
Recognising when muscle loss becomes clinically significant requires awareness of specific warning signs and symptoms. Whilst some lean tissue reduction during weight loss is expected, excessive or rapid muscle loss can compromise physical function, metabolic health, and quality of life.
Contact your GP if you experience:
Significant functional decline – difficulty performing previously manageable activities such as climbing stairs, rising from chairs, or carrying shopping
Unexplained weakness – progressive loss of strength disproportionate to weight loss achieved
Frequent falls or balance problems – suggesting compromised muscle strength and coordination
Difficulty meeting protein targets – persistent nausea or early satiety preventing adequate nutritional intake
Rapid weight loss – exceeding 0.5–1 kg weekly consistently, which may indicate excessive muscle catabolism
Sarcopenic symptoms – visible muscle wasting, particularly in the thighs, upper arms, or shoulders
Seek urgent medical advice if you experience persistent vomiting, dehydration, or inability to maintain adequate fluid and nutrition intake.
Your GP can arrange appropriate investigations, including:
Functional assessments such as grip strength testing, sit-to-stand tests, or timed up-and-go tests
Body composition analysis using bioelectrical impedance where available (note that DEXA scanning for body composition is not routinely available on the NHS)
Nutritional review – referral to dietetic services for optimised meal planning
Blood tests – checking for nutritional deficiencies (vitamin D, B12, iron) that may compound muscle loss
Referral to specialist services may be appropriate for patients with:
Pre-existing sarcopenia or frailty
Significant comorbidities affecting muscle metabolism (chronic kidney disease, heart failure)
Age over 65 years with concerning functional decline
Inadequate response to initial muscle-preserving interventions
Regular monitoring throughout weight loss treatment enables early identification of concerning trends, allowing timely intervention to protect muscle mass whilst achieving beneficial fat loss. NICE guidance emphasises that weight management should improve overall health and function, not compromise it through excessive lean tissue depletion.
If you experience any suspected side effects from weight loss injections, report them through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Yes, muscle loss can be minimised through resistance training at least twice weekly, consuming 1.0–1.5 grams of protein per kilogram body weight daily, and avoiding excessively low-calorie diets. Research shows that combining GLP-1 medications with structured exercise programmes significantly improves lean mass preservation.
Clinical trials indicate that approximately 25–30% of weight lost during GLP-1 receptor agonist treatment comprises lean body mass, which includes muscle tissue, water, and bone. This proportion is similar to weight loss from other methods and can be reduced through appropriate protein intake and resistance training.
Contact your GP if you experience significant functional decline, difficulty performing daily activities, unexplained weakness, frequent falls, or visible muscle wasting. Your GP can arrange functional assessments, body composition analysis, and referral to dietetic or specialist services if needed.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.