The half-life of tirzepatide is approximately 5 days (around 120 hours), a pharmacokinetic property that enables once-weekly subcutaneous dosing for type 2 diabetes and weight management. This extended half-life results from molecular modifications that enhance albumin binding and resist enzymatic degradation. Understanding tirzepatide's half-life is essential for healthcare professionals and patients, as it influences dosing schedules, time to steady-state concentrations, management of missed doses, and the persistence of therapeutic effects after discontinuation. This article explores the clinical implications of tirzepatide's pharmacokinetics and how its prolonged elimination profile shapes treatment protocols in UK practice.
Quick Answer: Tirzepatide has a half-life of approximately 5 days (120 hours), enabling once-weekly subcutaneous administration.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereTirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It is also licensed for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, under the brand name Mounjaro. It represents the first dual incretin receptor agonist approved by the Medicines and Healthcare products Regulatory Agency (MHRA).
The drug works by simultaneously activating both GIP and GLP-1 receptors, which are naturally occurring incretin hormones involved in glucose homeostasis. GLP-1 receptor activation stimulates glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriate glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways. GIP receptor activation complements these effects by enhancing insulin secretion and is thought to influence fat metabolism and energy expenditure, though these mechanisms are still being fully elucidated.
This dual mechanism results in improved glycaemic control, with reductions in HbA1c levels, alongside significant weight loss—effects that have been demonstrated in the SURPASS clinical trial programme. Tirzepatide is administered as a once-weekly subcutaneous injection, typically starting at 2.5 mg and titrated upwards based on individual response and tolerability.
Patients prescribed tirzepatide should receive comprehensive education about injection technique, potential adverse effects (particularly gastrointestinal symptoms), and the importance of maintaining regular follow-up appointments. Important safety considerations include: risk of hypoglycaemia when combined with insulin or sulfonylureas (dose reductions of these medications may be needed); monitoring for signs of pancreatitis or gallbladder disease; and that tirzepatide is not indicated for type 1 diabetes or diabetic ketoacidosis. Tirzepatide is not recommended in pregnancy, during breastfeeding, or in patients with severe gastrointestinal disease.
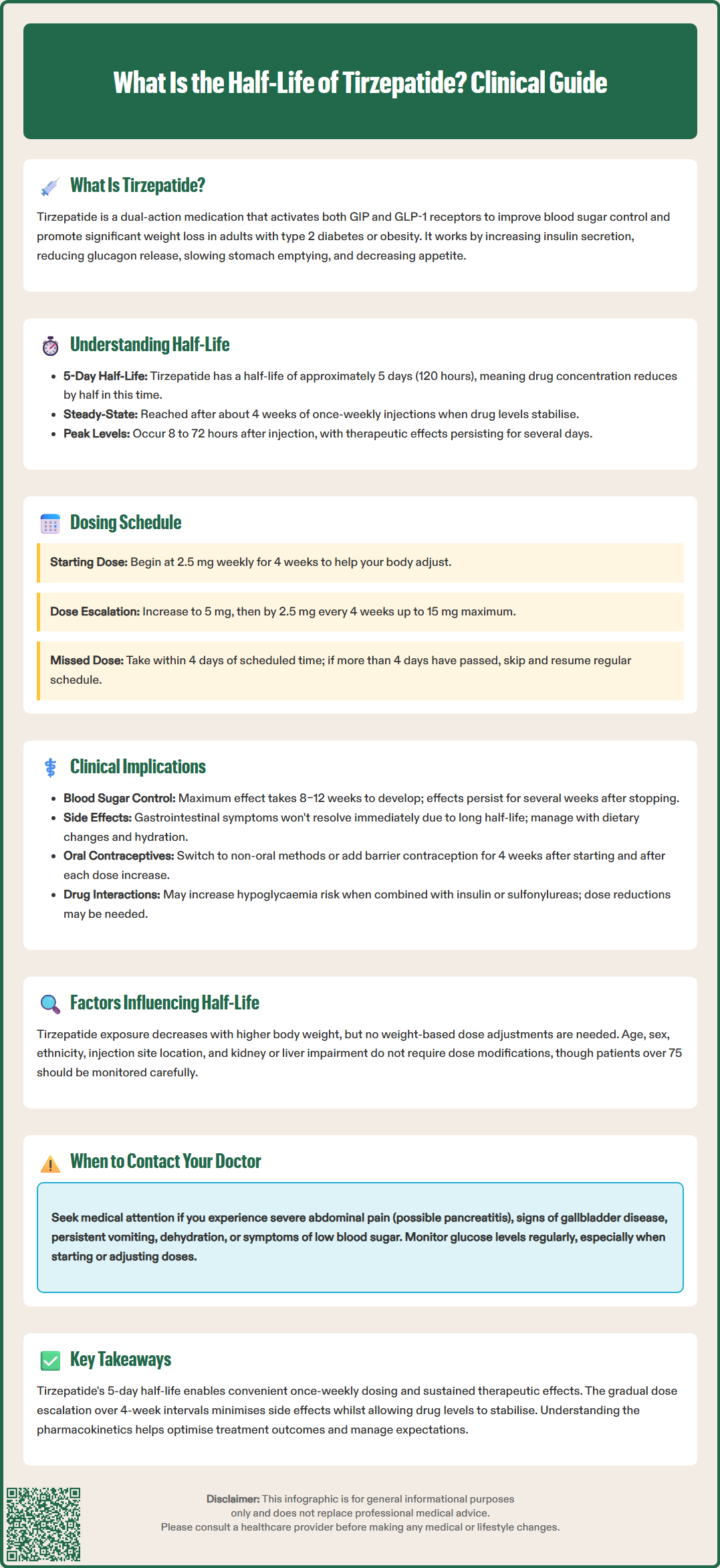
The half-life of tirzepatide is approximately 5 days (around 120 hours) following subcutaneous administration. This elimination half-life refers to the time required for the plasma concentration of the drug to decrease by half during the elimination phase. Understanding this concept is essential for both healthcare professionals and patients, as it directly influences dosing frequency, time to steady state, and the duration of therapeutic effect.
Tirzepatide's extended half-life is achieved through several molecular modifications to its peptide structure. The drug contains a C20 fatty diacid moiety that facilitates binding to albumin in the bloodstream, significantly prolonging its circulation time. Additionally, structural modifications provide resistance to degradation by dipeptidyl peptidase-4 (DPP-4), an enzyme that rapidly breaks down native incretin hormones. These design features transform what would otherwise be a rapidly cleared peptide into a long-acting therapeutic agent.
Following subcutaneous injection, tirzepatide is absorbed slowly from the injection site, with peak plasma concentrations typically occurring between 8 and 72 hours post-dose. Steady-state concentrations are achieved after approximately 4 weeks of once-weekly dosing, which corresponds to roughly four to five half-lives—a standard pharmacokinetic principle. At steady state, the amount of drug administered equals the amount eliminated during each dosing interval, resulting in consistent therapeutic levels.
The prolonged half-life means that tirzepatide remains active in the body for an extended period. Even if a dose is missed, therapeutic concentrations may persist for several days. According to the Summary of Product Characteristics (SmPC), if a dose is missed, it should be administered as soon as possible if within 4 days (96 hours) of the scheduled dose. If more than 4 days have passed, the missed dose should be skipped and the next dose administered on the regularly scheduled day.
The 5-day half-life of tirzepatide is the fundamental reason why it can be administered as a once-weekly subcutaneous injection, rather than requiring daily dosing like many other diabetes medications. This extended dosing interval offers practical advantages for patients by reducing the frequency of injections.
The standard dosing schedule begins with an initial dose of 2.5 mg once weekly for 4 weeks. This starting dose serves primarily as a tolerability step rather than a therapeutic dose, allowing the gastrointestinal system to adapt to the medication's effects on gastric emptying. After this initial period, the dose is increased to 5 mg once weekly, with further escalations in 2.5 mg increments every 4 weeks as needed, up to a maximum of 15 mg weekly for diabetes management. For weight management, the recommended maintenance doses are 5 mg, 10 mg, or 15 mg once weekly, depending on individual response and tolerability.
The 4-week intervals between dose escalations are carefully chosen based on tirzepatide's pharmacokinetics. As steady-state concentrations are reached after approximately 4 weeks, this timing ensures that each new dose level has achieved stable plasma concentrations before further increases are considered. This gradual titration approach minimises gastrointestinal adverse effects, which are the most common side effects associated with tirzepatide and other incretin-based therapies.
Patients should be advised to administer their weekly injection on the same day each week, though the time of day can vary. If a dose is missed, the SmPC advises: administer as soon as possible if within 4 days (96 hours) of the missed dose, then resume the regular weekly schedule. If more than 4 days have passed, skip the missed dose and administer the next dose on the regularly scheduled day. Patients should not take an extra dose to make up for a missed dose.
The pharmacokinetic profile of tirzepatide, particularly its extended half-life, has several important clinical implications for prescribers and patients. Understanding these factors enables optimised treatment outcomes and appropriate management of potential adverse effects or drug interactions.
Onset and offset of therapeutic effects are directly related to the drug's half-life. Whilst some glycaemic improvements may be observed within the first few weeks of treatment, maximal therapeutic effects typically develop gradually over 8–12 weeks as steady-state concentrations are achieved and maintained. Similarly, if treatment is discontinued, tirzepatide's effects will persist for several weeks as plasma concentrations decline. This extended offset period suggests that closer glucose monitoring may be appropriate for several weeks after discontinuation, particularly in patients with diabetes who may require alternative glucose-lowering therapy.
The long half-life also influences the management of adverse effects. Gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation are common, particularly during dose escalation. If these become intolerable, simply stopping the medication will not provide immediate relief, as therapeutic concentrations persist for days. Healthcare professionals should counsel patients about this possibility and provide symptomatic management strategies, including dietary modifications, antiemetic therapy if appropriate, and adequate hydration. Persistent severe vomiting may lead to dehydration and acute kidney injury, requiring prompt medical attention.
Drug interactions are generally limited with tirzepatide, but its effect on gastric emptying may influence the absorption of oral medications. According to the SmPC, for oral contraceptives, patients should use a non-oral contraceptive method or add a barrier method for 4 weeks after initiation and after each dose increase. For other medications with narrow therapeutic indices, careful monitoring may be appropriate.
Renal and hepatic impairment do not significantly affect tirzepatide pharmacokinetics, and dose adjustments are not required. However, patients should be monitored for signs of pancreatitis (severe abdominal pain, sometimes radiating to the back) and gallbladder disease. When used with insulin or sulfonylureas, there is an increased risk of hypoglycaemia, and dose reductions of these medications should be considered. Tirzepatide is not recommended in patients with severe gastrointestinal disease.
Suspected adverse reactions should be reported via the MHRA Yellow Card scheme.
Whilst tirzepatide exhibits relatively consistent pharmacokinetics across diverse patient populations, several factors warrant consideration as they may theoretically influence drug exposure, though clinical significance varies.
Body weight and composition have been evaluated in pharmacokinetic studies. Tirzepatide exposure (area under the concentration-time curve) decreases with increasing body weight, which is expected for a fixed-dose subcutaneous medication. However, the approved dosing regimen does not require weight-based adjustments, as the therapeutic dose range (5–15 mg weekly) has demonstrated efficacy across a broad spectrum of body weights in clinical trials. The drug's distribution is primarily to plasma and extracellular fluid, with albumin binding playing a key role in its prolonged circulation.
Age, sex, and ethnicity have been examined in population pharmacokinetic analyses. These demographic factors do not produce clinically meaningful differences in tirzepatide exposure that would necessitate dose modifications. Both male and female patients, across adult age ranges and various ethnic backgrounds, can be treated with standard dosing protocols. However, clinical experience in patients over 75 years is limited, and careful monitoring is advisable in elderly populations who may be more susceptible to adverse effects such as dehydration from gastrointestinal symptoms.
Renal and hepatic function do not significantly alter tirzepatide pharmacokinetics. The drug is presumed to undergo proteolytic degradation into smaller peptides and amino acids, similar to endogenous proteins, rather than traditional hepatic metabolism or renal excretion of intact drug. According to the SmPC, no dose adjustment is required for patients with renal impairment, including those with end-stage renal disease. Similarly, no dose adjustment is needed for patients with hepatic impairment. Nevertheless, patients with severe renal impairment or hepatic disease should be monitored for adverse effects, particularly if severe gastrointestinal symptoms lead to dehydration.
Injection site (abdomen, thigh, or upper arm) does not significantly affect the rate or extent of tirzepatide absorption, providing flexibility for patients to rotate injection sites to minimise local reactions. Patients should be educated to avoid injecting into areas of active skin disease, scarring, or lipohypertrophy, and to report any persistent injection site reactions to their healthcare provider.
With a half-life of approximately 5 days, tirzepatide remains active in the body for several weeks after the last dose. Therapeutic effects gradually decline as plasma concentrations decrease, with complete elimination taking several half-lives.
Tirzepatide's 5-day half-life allows once-weekly dosing because the drug remains at therapeutic concentrations throughout the week. This extended half-life results from molecular modifications that enhance albumin binding and resist enzymatic breakdown.
If you miss a dose, administer it as soon as possible if within 4 days (96 hours) of the scheduled dose, then resume your regular weekly schedule. If more than 4 days have passed, skip the missed dose and take the next dose on your regularly scheduled day.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.