
Metabolic imbalance refers to disruptions in the body's biochemical processes that convert food into energy and maintain cellular function. Rather than a single diagnosis, it encompasses various conditions including electrolyte disturbances, acid-base disorders, glucose metabolism problems, and lipid abnormalities. These imbalances can affect multiple organ systems, particularly the endocrine system, liver, and kidneys. Early detection through routine blood tests—such as urea and electrolytes, liver function, thyroid function, HbA1c, and lipid profiles—enables timely intervention. Understanding the causes, symptoms, and management options is essential for preventing complications and restoring metabolic equilibrium.
Quick Answer: Metabolic imbalance describes disruptions in the body's biochemical processes that regulate energy production and cellular function, encompassing conditions such as electrolyte disturbances, glucose metabolism problems, and hormonal dysregulation.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMetabolic imbalance is a descriptive umbrella term rather than a formal medical diagnosis. It refers to a disruption in the body's normal biochemical processes that convert food into energy and maintain cellular function. Metabolism encompasses thousands of chemical reactions occurring continuously within cells, regulated by enzymes, hormones, and various organ systems. When these processes become dysregulated, the body may struggle to maintain homeostasis—the stable internal environment necessary for optimal health.
This broad concept can encompass several distinct conditions. These include electrolyte disturbances (such as abnormal sodium, potassium, or calcium levels), acid-base disorders (where blood pH becomes too acidic or alkaline), glucose metabolism problems (including diabetes and hypoglycaemia), and lipid abnormalities (such as dyslipidaemia). Additionally, inherited metabolic disorders—though rarer—represent genetic defects in specific metabolic pathways.
Metabolic syndrome is a specific, defined cluster of conditions including central obesity, dyslipidaemia, hypertension and raised glucose levels, which together increase cardiometabolic risk.
Metabolic imbalances can affect multiple organ systems simultaneously. The endocrine system, particularly the thyroid, pancreas, and adrenal glands, plays a central role in metabolic regulation. The liver and kidneys are equally crucial, as they process nutrients, eliminate waste products, and maintain electrolyte balance. When any of these systems malfunction, cascading effects can occur throughout the body.
Early identification through routine blood tests (such as urea and electrolytes, liver function tests, thyroid function, HbA1c, and lipid profiles) can detect abnormalities before symptoms develop. Appropriate management is essential to prevent complications and restore metabolic equilibrium.
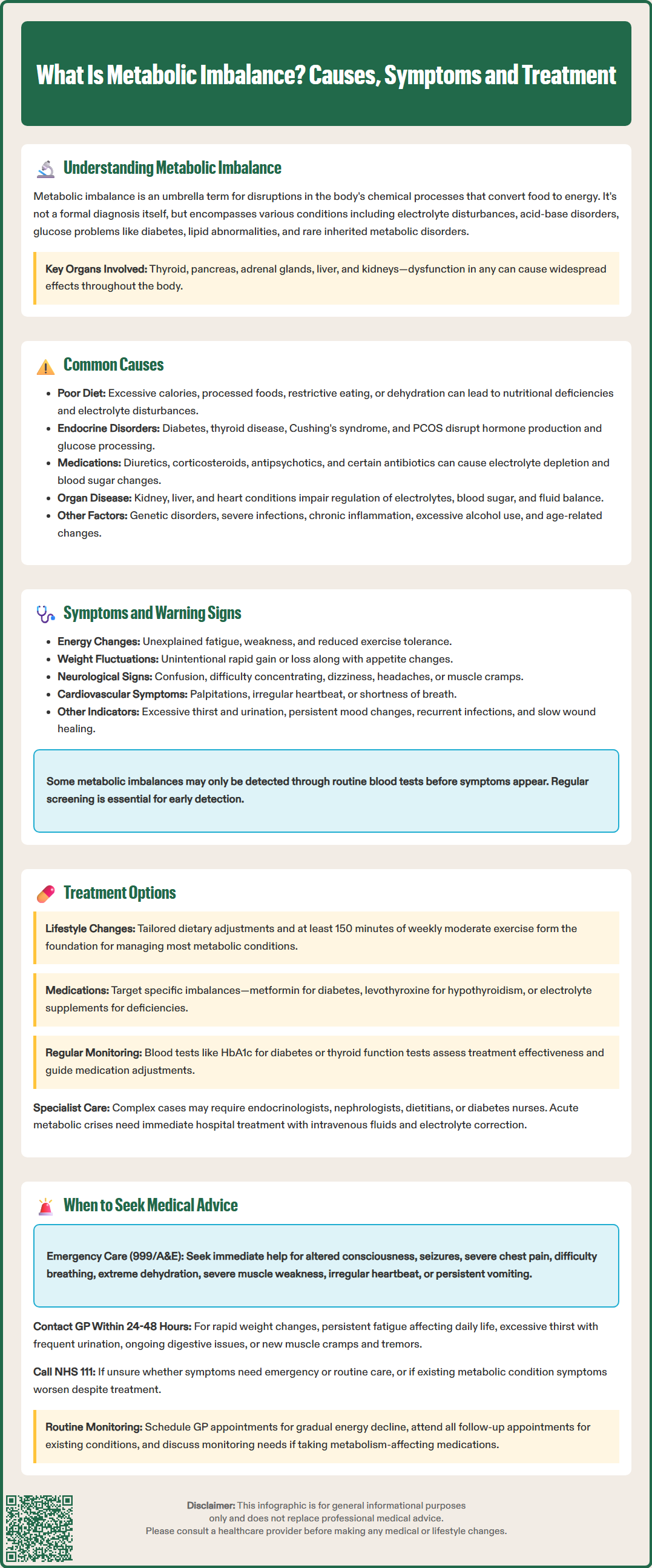
Metabolic imbalances arise from numerous underlying causes, ranging from lifestyle factors to serious medical conditions. Dietary factors represent one of the most common contributors. Inadequate nutrition, excessive calorie intake, high consumption of processed foods, or restrictive dieting can all disrupt normal metabolic function. Severe dietary restriction may lead to nutritional deficiencies, electrolyte disturbances, and in extreme cases, refeeding syndrome when nutrition is reintroduced. Dehydration similarly affects electrolyte balance and cellular metabolism, particularly during illness or intense physical activity.
Endocrine disorders are significant causes of metabolic dysfunction. Diabetes mellitus, both type 1 and type 2, disrupts glucose metabolism through insufficient insulin production or insulin resistance. Thyroid disorders—including hypothyroidism and hyperthyroidism—alter metabolic rate, affecting how the body uses energy. Cushing's syndrome, Addison's disease, and polycystic ovary syndrome (PCOS) also create metabolic disturbances through hormonal dysregulation.
Medications can inadvertently cause metabolic imbalances. Loop and thiazide diuretics may deplete potassium and sodium; corticosteroids affect glucose metabolism and can induce hyperglycaemia; second-generation antipsychotics are associated with weight gain and metabolic syndrome. Specific antibiotics can cause electrolyte disturbances (e.g., trimethoprim-associated hyperkalaemia). Chemotherapy agents and immunosuppressants can also disrupt normal metabolic processes.
Organ dysfunction frequently underlies metabolic problems. Chronic kidney disease impairs the body's ability to regulate electrolytes, fluid balance, and acid-base status. Liver disease affects glucose regulation, protein synthesis, and toxin elimination. Heart failure can lead to fluid retention and electrolyte abnormalities.
Other causes include genetic metabolic disorders (such as phenylketonuria or glycogen storage diseases), acute illnesses (including severe infections or sepsis), chronic inflammatory conditions, and excessive alcohol consumption. Age-related changes in metabolism, particularly during menopause or with advancing age, can also contribute to metabolic dysregulation. Identifying the underlying cause is essential for targeted treatment.
The symptoms of metabolic imbalance vary considerably depending on which metabolic processes are affected and the severity of the disruption. However, certain warning signs should prompt medical evaluation. Unexplained fatigue is one of the most common presentations, often accompanied by weakness and reduced exercise tolerance. This occurs because cells cannot efficiently produce or utilise energy when metabolic pathways are compromised.
Changes in weight without intentional dietary modification warrant attention. Rapid weight gain may indicate fluid retention, hormonal imbalances, or conditions like hypothyroidism. Conversely, unexplained weight loss can signal hyperthyroidism, uncontrolled diabetes, or malabsorption disorders. Changes in appetite—either increased hunger or loss of appetite—often accompany metabolic disturbances.
Neurological symptoms frequently manifest with metabolic imbalances, particularly electrolyte abnormalities. These may include confusion, difficulty concentrating, memory problems, dizziness, headaches, or in severe cases, seizures or altered consciousness. Muscle symptoms such as cramps, weakness, tremors, or abnormal sensations (paraesthesia) can indicate electrolyte disturbances, particularly involving potassium, calcium, or magnesium.
Cardiovascular symptoms including palpitations, irregular heartbeat, chest discomfort, or shortness of breath may occur with certain metabolic imbalances. Electrolyte abnormalities can affect cardiac rhythm, whilst thyroid disorders alter heart rate and function. Gastrointestinal symptoms—nausea, vomiting, constipation, or diarrhoea—are common with various metabolic disturbances.
Diabetic emergencies may present with specific symptoms including very high glucose with ketones, vomiting, abdominal pain, and rapid breathing. Severe electrolyte disturbances can cause new-onset confusion, seizures, or arrhythmias.
Other warning signs include excessive thirst and urination (suggesting diabetes or electrolyte problems), persistent mood changes, sleep disturbances, recurrent infections, slow wound healing, and changes in skin, hair, or nail condition. The presence of multiple symptoms, particularly if progressive or severe, necessitates prompt medical assessment. It is important to note that symptoms can be subtle initially, and some individuals may have metabolic abnormalities detected only through routine blood tests before symptoms develop.
Treatment of metabolic imbalance must address the underlying cause whilst managing symptoms and preventing complications. The approach is highly individualised, depending on the specific metabolic disturbance identified. Lifestyle modifications form the foundation of management for many metabolic conditions. Dietary adjustments tailored to the specific imbalance are crucial—this may involve carbohydrate management for diabetes, potassium restriction for hyperkalaemia, or balanced nutrition to address deficiencies.
Regular physical activity improves insulin sensitivity, aids weight management, and enhances overall metabolic function. The UK Chief Medical Officers and NHS recommend at least 150 minutes of moderate-intensity activity weekly for adults. However, exercise programmes should be individualised, particularly for those with significant comorbidities.
Pharmacological interventions target specific metabolic abnormalities. For diabetes, medications range from metformin (which reduces hepatic glucose production and improves insulin sensitivity) to insulin therapy for those requiring it. Thyroid disorders require hormone replacement (levothyroxine for hypothyroidism) or antithyroid medications (such as carbimazole for hyperthyroidism). Electrolyte imbalances may necessitate supplementation or medications that help retain or excrete specific electrolytes.
Monitoring and adjustment are essential components of management. Regular blood tests assess metabolic parameters, allowing treatment optimisation. For diabetes, this includes HbA1c monitoring; for thyroid disorders, thyroid function tests guide dose adjustments. Patients may require education on self-monitoring, such as blood glucose testing.
Specialist input may be necessary for complex cases. Endocrinologists manage hormonal disorders, whilst nephrologists address kidney-related metabolic problems. Dietitians provide expert nutritional guidance, and diabetes specialist nurses offer education and support for glucose management.
For inherited metabolic disorders, treatment may involve enzyme replacement therapy, dietary restrictions of specific substances, or supplementation with cofactors. Acute metabolic crises require hospital admission for intravenous fluid and electrolyte correction, close monitoring, and treatment of precipitating factors. The goal of all interventions is to restore metabolic balance, prevent complications, and optimise quality of life whilst addressing the root cause of the imbalance.
If you experience side effects from any medication, report them to your healthcare professional and through the MHRA Yellow Card scheme.
Knowing when to seek medical attention for potential metabolic imbalance is crucial for preventing serious complications. Immediate medical attention (via 999 or attending A&E) is necessary if you experience severe symptoms including altered consciousness, confusion, seizures, severe chest pain, difficulty breathing, or signs of severe dehydration (such as minimal urine output, extreme thirst, or dizziness upon standing).
Severe muscle weakness that impairs movement, irregular or very rapid heartbeat, or persistent vomiting preventing fluid intake also warrant emergency assessment. These symptoms may indicate life-threatening metabolic disturbances requiring urgent correction.
Contact your GP promptly (within 24-48 hours) if you notice rapid or unintentional weight changes, persistent fatigue that interferes with daily activities, excessive thirst accompanied by frequent urination, or ongoing gastrointestinal symptoms. New or worsening muscle cramps, tremors, or abnormal sensations should also prompt medical review.
If you're unsure whether your symptoms require A&E attendance or GP review, contact NHS 111 for advice. This service can help determine the appropriate level of care needed.
If you have a diagnosed metabolic condition, seek advice when symptoms worsen despite treatment, when you experience side effects from medications, or if you're unable to maintain your usual management routine due to illness. Pregnant women should be particularly vigilant and contact their maternity unit or triage service for urgent concerns, as metabolic changes during pregnancy require careful monitoring.
Routine medical review is appropriate for subtler concerns such as gradual energy decline, mild mood changes, or general concerns about metabolic health. Your GP can arrange appropriate blood tests to assess metabolic function, including glucose levels, electrolytes, kidney and liver function, and thyroid hormones.
For those with existing metabolic conditions, attend all scheduled follow-up appointments and monitoring tests. Regular review allows early detection of deterioration and treatment adjustment before complications develop. If you're taking medications that can affect metabolism, discuss monitoring requirements with your GP or pharmacist. Remember that early intervention for metabolic imbalances typically leads to better outcomes and can prevent progression to more serious conditions.
Common symptoms include unexplained fatigue, unintentional weight changes, muscle weakness or cramps, confusion or difficulty concentrating, and changes in appetite. Cardiovascular symptoms such as palpitations and gastrointestinal disturbances may also occur depending on which metabolic processes are affected.
Many metabolic imbalances respond well to lifestyle modifications including dietary adjustments, regular physical activity, and adequate hydration. However, treatment depends on the underlying cause; some conditions require medication or specialist intervention alongside lifestyle changes.
Diagnosis involves routine blood tests including urea and electrolytes, liver function tests, thyroid function, HbA1c, and lipid profiles. Your GP will assess symptoms, medical history, and test results to identify specific metabolic abnormalities and determine appropriate management.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.