Rybelsus (semaglutide) represents a significant therapeutic advance as the first oral glucagon-like peptide-1 receptor agonist (GLP-1 RA) for type 2 diabetes mellitus. Despite its innovative delivery system and proven efficacy in reducing HbA1c and body weight, Rybelsus has not achieved widespread adoption in UK clinical practice. Multiple factors contribute to its limited popularity, including substantial cost compared to established oral antidiabetic agents, restrictive NICE prescribing criteria, complex dosing requirements, and intermittent supply constraints. Understanding these barriers is essential for clinicians and patients considering this treatment option within the context of personalised diabetes management.
Quick Answer: Rybelsus remains less popular primarily due to high cost, restrictive NICE prescribing criteria, complex dosing requirements, and intermittent supply constraints within the NHS.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereRybelsus (semaglutide) is the first oral formulation of a glucagon-like peptide-1 receptor agonist (GLP-1 RA) licensed for the treatment of type 2 diabetes mellitus in adults to improve glycaemic control. It received European Medicines Agency (EMA) central authorisation and became available in the UK in 2020. Importantly, Rybelsus is not indicated for type 1 diabetes, diabetic ketoacidosis, or for patients under 18 years of age.
The active ingredient, semaglutide, mimics the action of endogenous GLP-1, a naturally occurring incretin hormone. Its mechanism of action involves binding to GLP-1 receptors on pancreatic beta cells, which stimulates glucose-dependent insulin secretion. Simultaneously, it suppresses glucagon release from alpha cells, thereby reducing hepatic glucose production. Semaglutide also slows gastric emptying and promotes satiety through central nervous system pathways, contributing to weight reduction—a beneficial effect for many patients with type 2 diabetes who are overweight or obese.
Rybelsus is available in three tablet strengths: 3 mg, 7 mg, and 14 mg. The 3 mg dose serves as an initial titration step for 30 days to improve gastrointestinal tolerability, with patients then progressing to 7 mg. After at least another 30 days, escalation to 14 mg may be considered if additional glycaemic control is needed. The PIONEER clinical trial programme demonstrated that Rybelsus significantly reduces HbA1c levels (typically 1.0-1.4% reduction with 14 mg) and body weight compared to placebo and certain other oral antidiabetic agents.
Key safety considerations include risk of pancreatitis, diabetic retinopathy complications (particularly in patients on insulin), gallbladder disease, and contraindication during pregnancy and breastfeeding.
Despite its innovative oral delivery system and proven efficacy, Rybelsus has not achieved the widespread adoption that might have been anticipated. Understanding the factors limiting its popularity requires examination of prescribing patterns, access barriers, and practical considerations affecting both clinicians and patients.
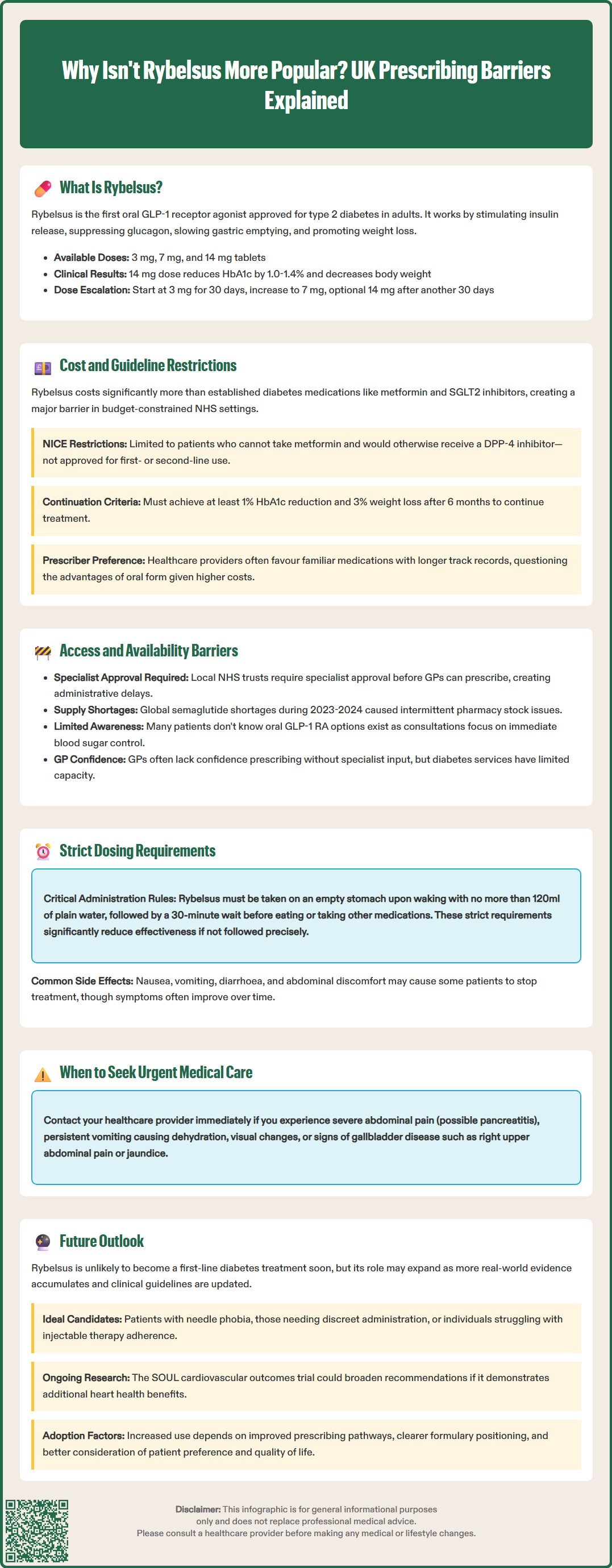
Several interconnected factors contribute to the relatively limited prescribing of Rybelsus within the UK healthcare system. Cost considerations represent a primary barrier. According to the British National Formulary (BNF), Rybelsus is substantially more expensive than established oral antidiabetic medications such as metformin, sulfonylureas, and even SGLT2 inhibitors. NHS England and local integrated care boards (ICBs) operate within constrained budgets, and prescribing decisions increasingly reflect cost-effectiveness analyses.
The National Institute for Health and Care Excellence (NICE) issued guidance (TA775, February 2022) recommending Rybelsus as an option for treating type 2 diabetes, but only under specific circumstances. NICE stipulates that semaglutide tablets are recommended when:
Metformin is contraindicated or not tolerated, and
A dipeptidyl peptidase-4 (DPP-4) inhibitor would otherwise be prescribed, and
A sulfonylurea or pioglitazone is not appropriate
These restrictive criteria mean Rybelsus occupies a narrow therapeutic niche rather than being positioned as a first- or second-line agent. Additionally, NICE guideline NG28 for type 2 diabetes management specifies that GLP-1 RAs should only be continued if patients achieve at least an 11 mmol/mol (1%) reduction in HbA1c and 3% weight loss after 6 months.
Clinical inertia also plays a role. Healthcare professionals may be more comfortable prescribing medications they have used extensively. Injectable GLP-1 RAs have a longer track record, and some diabetes specialists question whether the oral formulation offers sufficient advantages to justify the additional expense and prescribing complexity.
Furthermore, the COVID-19 pandemic disrupted routine diabetes care, with many medication reviews conducted remotely. This may have reduced opportunities to discuss newer treatment options like Rybelsus, particularly when existing therapies were providing adequate control.
Beyond prescribing patterns, structural and administrative barriers significantly impact patient access to Rybelsus. Many NHS trusts and ICBs have implemented local formulary restrictions, requiring specialist initiation or recommendation before GPs can prescribe Rybelsus. These additional administrative steps create delays and may discourage both clinicians and patients from pursuing this treatment option.
Pharmacy supply issues have periodically affected Rybelsus availability. Global demand for semaglutide products has resulted in supply constraints, as documented in NHS England supply disruption alerts during 2023-2024. When medications are intermittently unavailable, prescribers naturally gravitate towards more reliably stocked alternatives.
The commissioning landscape also influences access. Whilst Rybelsus is available on NHS prescription, some patients may encounter difficulties if their local ICB formulary classifications do not prioritise GLP-1 RA therapy or if pathways between primary and secondary care are unclear. Patients who do not meet NICE criteria may require individual funding requests (IFRs), which are rarely approved, and the medication's high cost makes private purchase prohibitive for most individuals.
Patient awareness represents another access barrier. Many people with type 2 diabetes are unaware that an oral GLP-1 RA exists. Healthcare consultations often focus on immediate glycaemic control rather than exploring the full range of available therapies. Without proactive discussion, patients may not know to ask about Rybelsus or understand how it differs from injectable alternatives.
Additionally, prescribing confidence varies among healthcare professionals. Some GPs may feel more comfortable initiating Rybelsus following specialist recommendation, but diabetes specialist services face significant capacity constraints, limiting the number of patients who can be comprehensively reviewed.
The unique dosing requirements of Rybelsus present practical challenges that may deter both prescribers and patients. Unlike most oral medications, Rybelsus must be taken under very specific conditions to ensure adequate absorption. Patients must:
Take the tablet on an empty stomach upon waking
Swallow it whole with no more than 120 ml of plain water
Wait at least 30 minutes before eating, drinking, or taking other oral medications
These stringent requirements can be difficult to integrate into daily routines, particularly for patients with complex medication regimens, shift workers, or those with unpredictable morning schedules. Non-adherence to these instructions significantly reduces semaglutide absorption and therapeutic efficacy.
Gastrointestinal adverse effects are common, especially during treatment initiation. Nausea, vomiting, diarrhoea, and abdominal discomfort affect a substantial proportion of patients. Whilst these symptoms often improve with continued use, some individuals discontinue treatment due to poor tolerability. The gradual dose escalation protocol (3 mg for 30 days, then 7 mg, with possible increase to 14 mg after at least another 30 days) aims to minimise these effects, but this means patients may wait several months before reaching a therapeutically optimal dose.
Patients should be advised to:
Stop treatment and seek urgent medical care if experiencing severe or persistent abdominal pain (potential pancreatitis)
Contact their healthcare provider for persistent vomiting leading to dehydration
Report visual changes or symptoms of diabetic retinopathy progression
Be aware of increased hypoglycaemia risk when used with insulin or sulfonylureas (dose adjustments may be needed)
Monitor for signs of gallbladder disease (right upper abdominal pain, jaundice)
Report suspected adverse reactions via the MHRA Yellow Card scheme
Interactions with other medications should be considered. Due to delayed gastric emptying, patients taking levothyroxine should have thyroid function monitored, as absorption may be affected.
Some patients find the oral formulation more acceptable than injections, representing Rybelsus's primary advantage. However, others may prefer the convenience of once-weekly injectable semaglutide (Ozempic) over daily oral administration with strict timing requirements. Individual preferences vary considerably, highlighting the importance of shared decision-making in diabetes management.
Several factors may influence Rybelsus's future adoption within UK clinical practice. Evolving clinical evidence continues to emerge. The PIONEER 6 cardiovascular outcomes trial demonstrated non-inferiority for major adverse cardiovascular events compared to placebo, while the larger dedicated SOUL cardiovascular outcomes trial is ongoing. If Rybelsus demonstrates additional benefits in these domains, clinical guidelines may broaden recommendations for its use.
Patent protection and manufacturing complexity will likely maintain current pricing for the foreseeable future. As a biological product with a specialised oral delivery system (SNAC technology), developing competitive alternatives presents significant challenges compared to conventional small-molecule medications.
The growing emphasis on personalised diabetes care may favour Rybelsus for specific patient populations. Individuals with needle phobia, those requiring discrete medication administration, or patients who have struggled with injectable therapy adherence may particularly benefit. As healthcare professionals become more familiar with oral GLP-1 RAs, prescribing confidence should increase.
Improved patient support resources and clearer pathways between primary and secondary care could enhance uptake. Simplified specialist recommendation processes and clearer local formulary positioning would reduce administrative barriers.
Based on current evidence, Rybelsus is unlikely to become a first-line diabetes therapy in the near future. However, its role may evolve as:
Real-world evidence accumulates
Clinicians gain experience with appropriate patient selection
NICE guidance is reviewed and potentially updated
Healthcare systems develop more nuanced approaches to cost-effectiveness that consider patient preference and quality of life
Ultimately, Rybelsus represents an important addition to the diabetes therapeutic armamentarium. Whilst current barriers limit its popularity, ongoing developments in clinical practice, health economics, and patient-centred care may gradually enhance its position in type 2 diabetes management strategies across the UK.
Rybelsus prescribing is limited primarily by high cost compared to other oral diabetes medications, restrictive NICE criteria requiring metformin unsuitability and specific alternative therapy considerations, and complex dosing requirements that affect patient adherence.
NICE recommends Rybelsus only when metformin is contraindicated or not tolerated, a DPP-4 inhibitor would otherwise be prescribed, and sulfonylureas or pioglitazone are inappropriate. Treatment should continue only if patients achieve at least 11 mmol/mol HbA1c reduction and 3% weight loss after six months.
Rybelsus must be taken on an empty stomach upon waking with no more than 120 ml of plain water, followed by a mandatory 30-minute wait before consuming food, beverages, or other oral medications. Non-adherence to these specific instructions significantly reduces therapeutic efficacy.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.