
Many people with type 2 diabetes wonder what HbA1c level is required to access Ozempic (semaglutide) through the NHS. In the UK, there is no single universal HbA1c threshold that automatically qualifies you for this medication. Instead, prescribing decisions follow NICE guidance and consider multiple factors including your current diabetes control, body mass index, existing treatments, and individual circumstances. Generally, NICE recommends GLP-1 receptor agonists like Ozempic when HbA1c remains at 58 mmol/mol (7.5%) or above despite dual therapy, alongside specific BMI criteria. This article explains the eligibility requirements, how HbA1c fits into prescribing decisions, and what to discuss with your GP.
Quick Answer: There is no single HbA1c threshold for Ozempic in the UK; NICE generally recommends GLP-1 receptor agonists when HbA1c remains at 58 mmol/mol (7.5%) or above despite dual therapy, alongside BMI and other clinical criteria.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a once-weekly injectable medication licensed in the UK for the treatment of type 2 diabetes mellitus. It belongs to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists, which mimic the action of a naturally occurring hormone that regulates blood glucose levels.
The mechanism of action involves several complementary pathways. Ozempic stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning it only promotes insulin release when blood sugar levels are elevated. This reduces the risk of hypoglycaemia compared to some other diabetes medications. Simultaneously, it suppresses glucagon secretion—a hormone that raises blood glucose—thereby preventing excessive glucose production by the liver.
Beyond glycaemic control, Ozempic slows gastric emptying, which helps moderate post-meal blood sugar spikes and promotes satiety. Many patients experience weight loss as a secondary benefit, which can further improve insulin sensitivity and overall metabolic health. Clinical trials have demonstrated that semaglutide significantly reduces HbA1c levels (a measure of average blood glucose over 2–3 months) and has cardiovascular benefits, including reduced risk of major adverse cardiovascular events in people with established cardiovascular disease.
Ozempic is administered subcutaneously once weekly using a pre-filled pen device. The dose is typically initiated at 0.25 mg weekly for 4 weeks, then increased to 0.5 mg. After at least 4 weeks at this dose, it may be increased to 1 mg weekly if needed, and after at least 4 further weeks, to 2 mg weekly for additional glycaemic control. It is important to note that Ozempic is not insulin and is not licensed for type 1 diabetes or diabetic ketoacidosis.
Patients should be aware of important safety considerations, including the risk of pancreatitis (seek urgent medical attention for severe, persistent abdominal pain), potential diabetic retinopathy complications (particularly with rapid improvement in blood glucose control), and increased risk of hypoglycaemia when used with insulin or sulfonylureas. Maintaining adequate hydration is important, especially if experiencing gastrointestinal side effects.
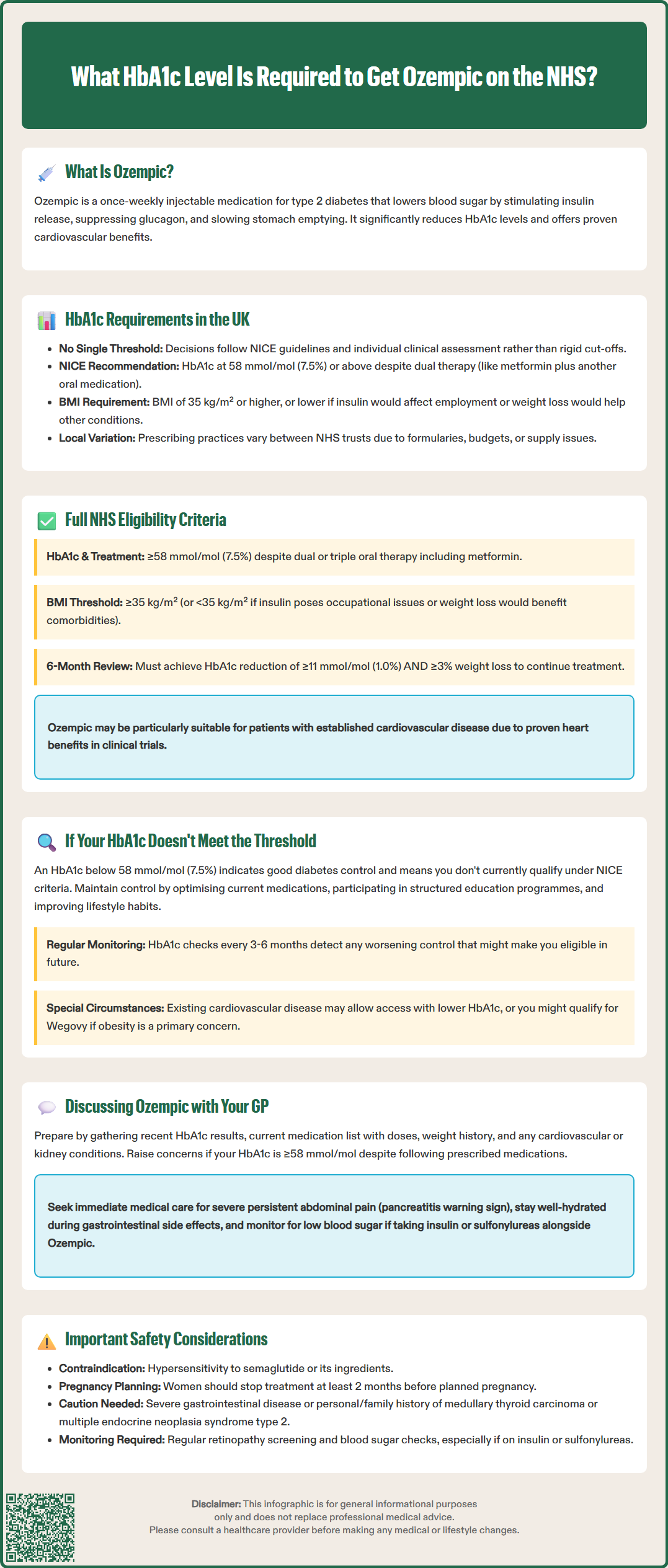
In the UK, there is no single, universal HbA1c threshold that definitively determines eligibility for Ozempic. Prescribing decisions are guided by NICE (National Institute for Health and Care Excellence) guidelines and individual clinical assessment rather than a rigid HbA1c cut-off alone.
NICE guidance (NG28) recommends GLP-1 receptor agonists like Ozempic for adults with type 2 diabetes when:
HbA1c levels remain at 58 mmol/mol (7.5%) or above despite treatment with dual therapy (typically metformin plus another oral agent), and
The patient has a body mass index (BMI) of 35 kg/m² or higher (adjusted accordingly for people from Black African, African-Caribbean and Asian family backgrounds), or
A BMI below 35 kg/m² where insulin therapy would have significant occupational implications or weight loss would benefit other significant obesity-related comorbidities.
These criteria reflect a holistic approach that considers not only glycaemic control but also weight, cardiovascular risk, and individual circumstances. The HbA1c threshold of 58 mmol/mol serves as a general benchmark indicating inadequate diabetes control on existing therapy, but clinical judgement remains paramount.
It is worth noting that prescribing practices may vary between NHS trusts and individual GPs, with some areas having local formularies or additional restrictions due to budget constraints or supply considerations. Private prescriptions may follow different criteria, though responsible clinicians still adhere to evidence-based guidelines. Patients should discuss their specific HbA1c results and overall diabetes management plan with their healthcare team to determine whether Ozempic is appropriate.
NHS eligibility for Ozempic extends beyond HbA1c levels and encompasses several clinical and practical considerations. According to NICE guidance NG28, GLP-1 receptor agonists are recommended as part of a comprehensive diabetes management strategy when specific conditions are met.
Primary eligibility criteria include:
Inadequate glycaemic control (HbA1c ≥58 mmol/mol or 7.5%) on dual or triple oral therapy, typically including metformin
BMI ≥35 kg/m² (adjusted accordingly for people from Black African, African-Caribbean and Asian family backgrounds)
Alternatively, BMI <35 kg/m² where insulin therapy poses occupational concerns or where weight loss would significantly benefit obesity-related comorbidities
Additionally, NICE recommends that treatment should only continue if there is a beneficial metabolic response, defined as:
A reduction in HbA1c of at least 11 mmol/mol (1.0%), and
Weight loss of at least 3% of initial body weight at 6 months
If these targets are not achieved, discontinuation should be considered. This ensures that NHS resources are directed toward patients who derive meaningful clinical benefit.
Cardiovascular considerations also influence prescribing. Ozempic has demonstrated cardiovascular benefits in clinical trials, and may be particularly appropriate for patients with type 2 diabetes and established cardiovascular disease, within NICE guidance and local formulary policies.
Patients must also be willing and able to self-inject weekly and attend regular monitoring appointments. The only formal contraindication in the UK is hypersensitivity to semaglutide or any excipients. However, Ozempic is not recommended during pregnancy or breastfeeding (women should discontinue treatment at least 2 months before a planned pregnancy), and should be used with caution in patients with severe gastrointestinal disease. Patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2 should discuss these conditions with their healthcare provider before starting treatment.
If your HbA1c is below 58 mmol/mol (7.5%), you may not currently meet NICE criteria for Ozempic on the NHS, but this does not mean your diabetes management is inadequate or that you have no options. An HbA1c below this threshold generally indicates good glycaemic control, which is the primary goal of diabetes treatment.
Alternative management strategies include:
Optimising existing oral medications: Your GP may adjust doses of metformin, SGLT2 inhibitors, DPP-4 inhibitors, or sulfonylureas to maintain control
Lifestyle modifications: Structured education programmes (such as DESMOND), dietary changes, increased physical activity, and weight management remain cornerstone interventions
Regular monitoring: HbA1c should be checked every 3–6 months to ensure continued control and detect any deterioration early
If your HbA1c subsequently rises above the threshold despite optimised oral therapy, you may then become eligible for Ozempic or another GLP-1 receptor agonist. It is important to maintain regular contact with your diabetes care team and report any difficulties with blood sugar control, medication side effects, or lifestyle adherence.
Special circumstances may warrant consideration of GLP-1 therapy even with lower HbA1c levels. For example, if you have established cardiovascular disease, your specialist might recommend semaglutide in line with NICE guidance and local formulary policies. Similarly, if you are struggling with obesity-related complications, your clinician might explore other semaglutide formulations (such as Wegovy, licensed specifically for weight management) or alternative weight-loss interventions.
Private prescription is another option, though costs can be substantial and vary considerably. Patients considering this route should ensure they receive appropriate medical supervision, including baseline investigations, regular monitoring (including diabetic retinopathy screening), and management of any adverse effects.
Approaching your GP about Ozempic requires preparation and an understanding of the clinical context. A productive consultation focuses on your overall diabetes management, treatment goals, and whether Ozempic aligns with evidence-based guidelines.
Before your appointment:
Review your recent HbA1c results and bring a record of your blood glucose monitoring if you perform home testing
List your current medications, including doses and any side effects you have experienced
Document your weight history and any previous attempts at weight management
Note any cardiovascular conditions, kidney function results, or other relevant comorbidities
Prepare questions about treatment options, expected benefits, potential side effects, and monitoring requirements
During the consultation, explain your concerns about diabetes control and ask whether your current treatment plan is optimal. If your HbA1c is ≥58 mmol/mol despite adherence to prescribed medications, this is a key point to raise. Discuss whether you meet NICE criteria for GLP-1 therapy, including BMI thresholds and any occupational or comorbidity considerations.
Be open about your treatment preferences and concerns. Some patients worry about injections, while others are motivated by potential weight loss or cardiovascular benefits. Your GP can explain the practical aspects of Ozempic use, including injection technique, storage, and managing common side effects such as nausea.
Discuss important safety information, including warning signs of pancreatitis (severe, persistent abdominal pain), the need for retinopathy monitoring with rapid HbA1c improvement, and increased hypoglycaemia risk if you take sulfonylureas or insulin. Ask about reporting any suspected side effects through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
If your GP determines you are not currently eligible, ask about alternative strategies and what would need to change for you to qualify in future. Request a review timeline—typically 3–6 months—to reassess your HbA1c and overall control.
If there is disagreement about eligibility or you feel your concerns have not been adequately addressed, you may request a referral to a diabetes specialist or endocrinologist for a second opinion. Remember that prescribing decisions balance individual clinical need with NHS resources and evidence-based guidelines, and your GP is working within this framework to provide safe, effective care.
Generally, NICE criteria require HbA1c of 58 mmol/mol or above for NHS prescribing, though special circumstances such as established cardiovascular disease may warrant specialist consideration. An HbA1c below this threshold typically indicates good glycaemic control.
NHS eligibility also considers BMI (generally ≥35 kg/m², adjusted for ethnicity), inadequate control on dual therapy, occupational implications of insulin, and obesity-related comorbidities. Treatment continuation requires demonstrating HbA1c reduction of at least 11 mmol/mol and 3% weight loss at 6 months.
HbA1c should typically be checked every 3–6 months to monitor diabetes control and assess whether treatment adjustments are needed. A 6-month review is particularly important to evaluate whether Ozempic is producing the required metabolic response for continued NHS prescribing.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.