
If you're taking Ozempic (semaglutide) and facing surgery, understanding how this medication interacts with anaesthesia is essential for your safety. Ozempic, a GLP-1 receptor agonist used for type 2 diabetes management in the UK, slows gastric emptying—a mechanism that aids blood glucose control but may affect anaesthetic risk. Current UK guidance from the Association of Anaesthetists and Centre for Perioperative Care emphasises individualised risk assessment rather than routine medication discontinuation. This article explains the key anaesthetic considerations, pre-operative preparations, and when to discuss Ozempic management with your surgical team to ensure safe perioperative care whilst maintaining optimal diabetes control.
Quick Answer: Patients taking Ozempic should inform their anaesthetist before surgery, as the medication delays gastric emptying and may increase aspiration risk, requiring individualised risk assessment and potential safety modifications.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for type 2 diabetes management. Wegovy (also semaglutide) is the licensed product for weight management. These medications offer significant metabolic benefits but present important considerations for patients undergoing surgical procedures requiring anaesthesia.
The primary concern relates to delayed gastric emptying, a known pharmacological effect of GLP-1 medications. Semaglutide slows the movement of food through the digestive system, which normally aids glycaemic control and promotes satiety. This mechanism may result in retained gastric contents even after appropriate fasting periods before surgery in some patients, particularly those with additional risk factors. This potentially increases the risk of pulmonary aspiration during anaesthesia induction—a complication where stomach contents enter the lungs.
Guidance from UK anaesthetic bodies, including the Association of Anaesthetists and the Centre for Perioperative Care (CPOC), emphasises the importance of discussing GLP-1 medications with your surgical team well in advance of any planned procedure. Current UK practice increasingly favours an individualised, risk-stratified approach rather than routine discontinuation for all patients.
Patients taking Ozempic should inform their GP, surgeon, and anaesthetist about their medication during pre-operative assessments. This allows the clinical team to implement appropriate safety measures based on individual risk assessment, local protocols, and the specific procedure planned. Understanding these considerations helps ensure your surgery proceeds safely whilst maintaining optimal diabetes management throughout the perioperative period.
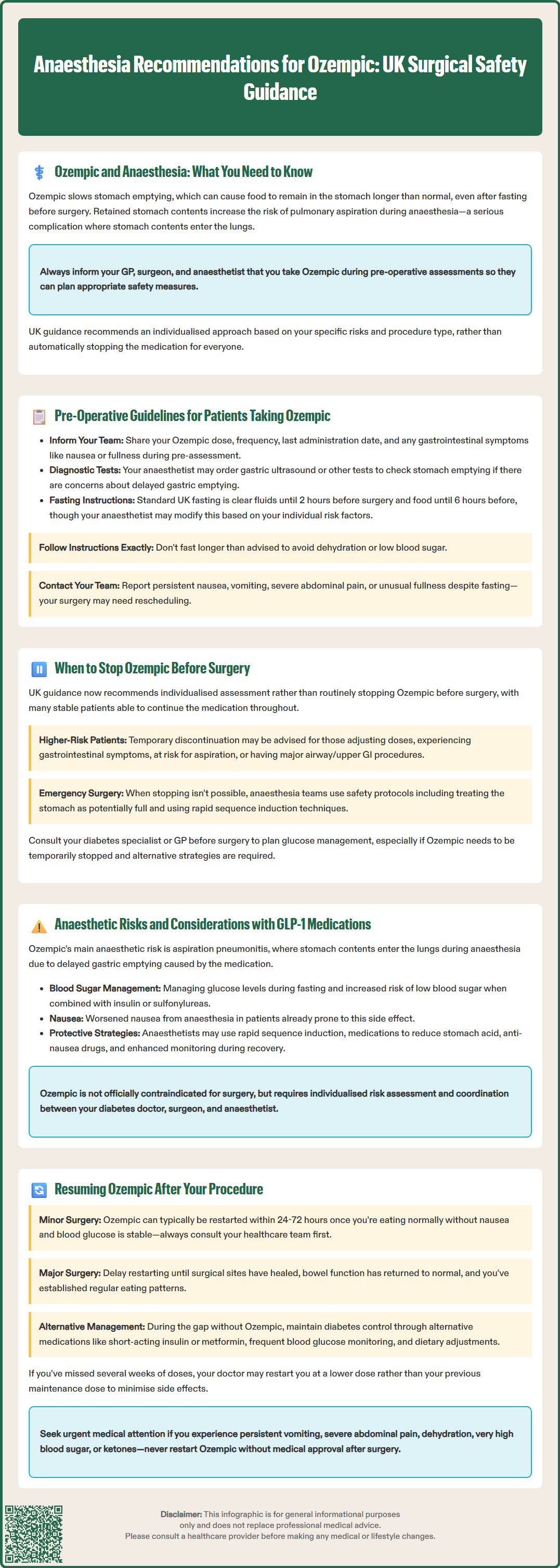
Comprehensive pre-operative assessment is essential for patients taking Ozempic. Your surgical team will need detailed information about your medication regimen, including the dose, frequency, and when you last administered Ozempic. The standard dosing schedule is once weekly, but individual timing varies.
During your pre-assessment appointment, expect questions about:
Your current Ozempic dose (typically 0.25 mg, 0.5 mg, 1 mg, or 2 mg weekly)
How long you have been taking the medication
Any gastrointestinal symptoms, particularly nausea, vomiting, or feeling of fullness
Your diabetes control and recent HbA1c levels
Other medications, especially those affecting gastric motility
Your anaesthetist may recommend additional investigations if there are concerns about gastric emptying. In some centres, point-of-care gastric ultrasound may be performed on the day of surgery to assess stomach contents, though availability varies across the UK and interpretation depends on operator experience.
Standard UK fasting guidance for adults typically allows clear fluids up to two hours before anaesthesia and food six hours prior, as recommended by the Association of Anaesthetists. For some patients on GLP-1 medications with additional risk factors (such as active gastrointestinal symptoms or known gastroparesis), your anaesthetist may recommend modified fasting instructions based on individual assessment.
It is crucial to follow your specific instructions precisely. Do not extend fasting beyond what is recommended, as this may lead to dehydration or hypoglycaemia. If you experience persistent nausea, vomiting, severe abdominal pain, or feel unusually full despite fasting, contact your surgical team immediately, as your procedure may need to be rescheduled. Never stop Ozempic without medical guidance, as this could affect your diabetes control.
The approach to Ozempic management before surgery is evolving, with UK practice increasingly favouring individualised risk assessment rather than routine discontinuation for all patients. Current UK guidance, including recommendations from the UK Clinical Pharmacy Association (UKCPA) Perioperative Medicines Handbook, suggests decisions should be made on a case-by-case basis.
For elective (planned) procedures, considerations include:
Many patients can continue Ozempic throughout the perioperative period, particularly those on stable doses without gastrointestinal symptoms
Temporary discontinuation may be considered for higher-risk patients, including those:
If your clinical team recommends temporarily stopping Ozempic, this should be done in consultation with your diabetes team to ensure appropriate glycaemic management during the perioperative period.
For emergency or urgent surgery, stopping Ozempic in advance is not possible. In these situations, your anaesthetic team will implement appropriate safety measures based on clinical assessment, which may include:
Treating as a potentially full stomach
Considering rapid sequence induction techniques
Considering use of medications to reduce gastric acidity
Potentially performing gastric ultrasound assessment where available
Patients should consult their diabetes specialist or GP about perioperative diabetes management. If Ozempic is temporarily withheld, alternative glucose management strategies will be needed. Your healthcare team will provide individualised advice based on your surgical timeline, diabetes control, and overall health status. Always document the date of your last Ozempic dose and inform your anaesthetist on the day of surgery.
Understanding the specific anaesthetic risks associated with Ozempic helps patients and clinicians make informed decisions about perioperative management. The primary concern centres on aspiration pneumonitis—a serious complication where acidic gastric contents enter the lungs during anaesthesia, potentially causing chemical injury, infection, and respiratory compromise.
GLP-1 receptor agonists like semaglutide exert their effect by mimicking the natural incretin hormone, which slows gastric emptying as part of its glucose-lowering mechanism. Some studies suggest patients taking these medications may have delayed gastric emptying, though the clinical significance varies between individuals and depends on factors such as dose, duration of treatment, and presence of other risk factors.
Additional anaesthetic considerations include:
Airway management: Obesity, if present, may influence airway assessment and management
Glycaemic control: Maintaining stable blood glucose levels perioperatively
Hypoglycaemia risk: Primarily when Ozempic is combined with insulin or sulfonylureas, particularly during fasting
Postoperative nausea and vomiting: Baseline nausea from Ozempic may be exacerbated by anaesthetic agents
Your anaesthetist may employ risk mitigation strategies based on individual assessment, which might include:
Consideration of rapid sequence induction in high-risk cases
Use of proton pump inhibitors or H2-receptor antagonists to reduce gastric acidity
Antiemetic prophylaxis
Appropriate airway management techniques
Enhanced monitoring during emergence from anaesthesia
There is no official contraindication to anaesthesia in patients taking Ozempic, but individualised risk assessment is essential. Patients with additional risk factors require particularly careful evaluation. Open communication between your diabetes team, surgeon, and anaesthetist ensures coordinated, safe perioperative care.
If you experience severe persistent abdominal pain, vomiting, or dehydration before or after surgery, seek urgent medical advice, as these could indicate serious complications requiring immediate assessment.
Restarting Ozempic following surgery requires careful consideration of several factors, including the type of procedure performed, your recovery progress, gastrointestinal function, and diabetes management needs. There is currently no universal protocol, and decisions should be individualised in consultation with your healthcare team.
For minor procedures with rapid recovery and minimal gastrointestinal impact, Ozempic may typically be resumed:
Once you are tolerating normal oral intake without significant nausea or vomiting
Often within 24-72 hours post-procedure, aligned with your regular weekly dosing schedule
When your blood glucose levels are stable
After discussion with your surgical and diabetes teams
Following major abdominal or gastrointestinal surgery, a more cautious approach is warranted. Your surgeon may recommend delaying Ozempic restart to allow:
Appropriate healing of surgical anastomoses (joined tissues)
Resolution of post-operative ileus (temporary bowel paralysis)
Establishment of normal eating patterns
Assessment of any ongoing gastrointestinal symptoms
Diabetes management during the gap period is crucial. Your GP or diabetes specialist may recommend:
Temporary use of alternative medications (e.g., short-acting insulin, metformin)
More frequent blood glucose monitoring
Dietary modifications to maintain glycaemic control
Regular follow-up to assess when Ozempic can safely resume
If you have missed doses for several weeks, your clinician may recommend following the SmPC guidance for missed doses, which may include restarting at a lower dose in some circumstances.
Contact your GP or diabetes team urgently if you experience persistent nausea, vomiting, severe abdominal pain, dehydration, significantly elevated blood glucose levels, or the presence of ketones. Never restart Ozempic without medical guidance, and ensure your diabetes team is aware of your surgical history when planning your medication restart.
If you experience any suspected side effects from Ozempic, report them to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
The decision to stop Ozempic before surgery should be individualised based on your specific risk factors, procedure type, and clinical assessment. Current UK guidance favours case-by-case evaluation rather than routine discontinuation, with many patients able to continue Ozempic throughout the perioperative period under appropriate monitoring.
Ozempic slows gastric emptying as part of its glucose-lowering mechanism, which may result in retained stomach contents even after appropriate fasting. This potentially increases the risk of pulmonary aspiration during anaesthesia induction, where gastric contents could enter the lungs.
Ozempic can typically be restarted once you are tolerating normal oral intake without significant nausea or vomiting, often within 24-72 hours after minor procedures. Following major abdominal or gastrointestinal surgery, your surgeon may recommend delaying restart to allow appropriate healing and resolution of post-operative gastrointestinal effects.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.