
Choosing the best fibre whilst on GLP-1 medications such as semaglutide (Ozempic, Wegovy) or liraglutide (Saxenda, Victoza) is essential for managing digestive side effects and optimising treatment outcomes. GLP-1 receptor agonists slow gastric emptying and reduce appetite, which can lead to constipation and other gastrointestinal symptoms. Incorporating appropriate dietary fibre—both soluble and insoluble types—helps maintain regular bowel function, stabilise blood glucose levels, and support overall gut health. This article explores evidence-based guidance on fibre intake for patients taking GLP-1 therapy, aligned with NHS and NICE recommendations, to improve tolerability and long-term adherence.
Quick Answer: The best fibre whilst on GLP-1 includes a balanced mix of soluble fibre (oats, chia seeds, beans, apples) and insoluble fibre (whole grains, vegetables, nuts) to prevent constipation and support digestive health.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists, such as semaglutide (Ozempic, Wegovy) and liraglutide (Saxenda, Victoza), have become increasingly prescribed for type 2 diabetes management and weight loss in the UK. These medications work by mimicking the natural GLP-1 hormone, which slows gastric emptying, reduces appetite, and improves glycaemic control. However, this mechanism of action can significantly affect digestive function, making dietary fibre an important consideration for patients on these therapies.
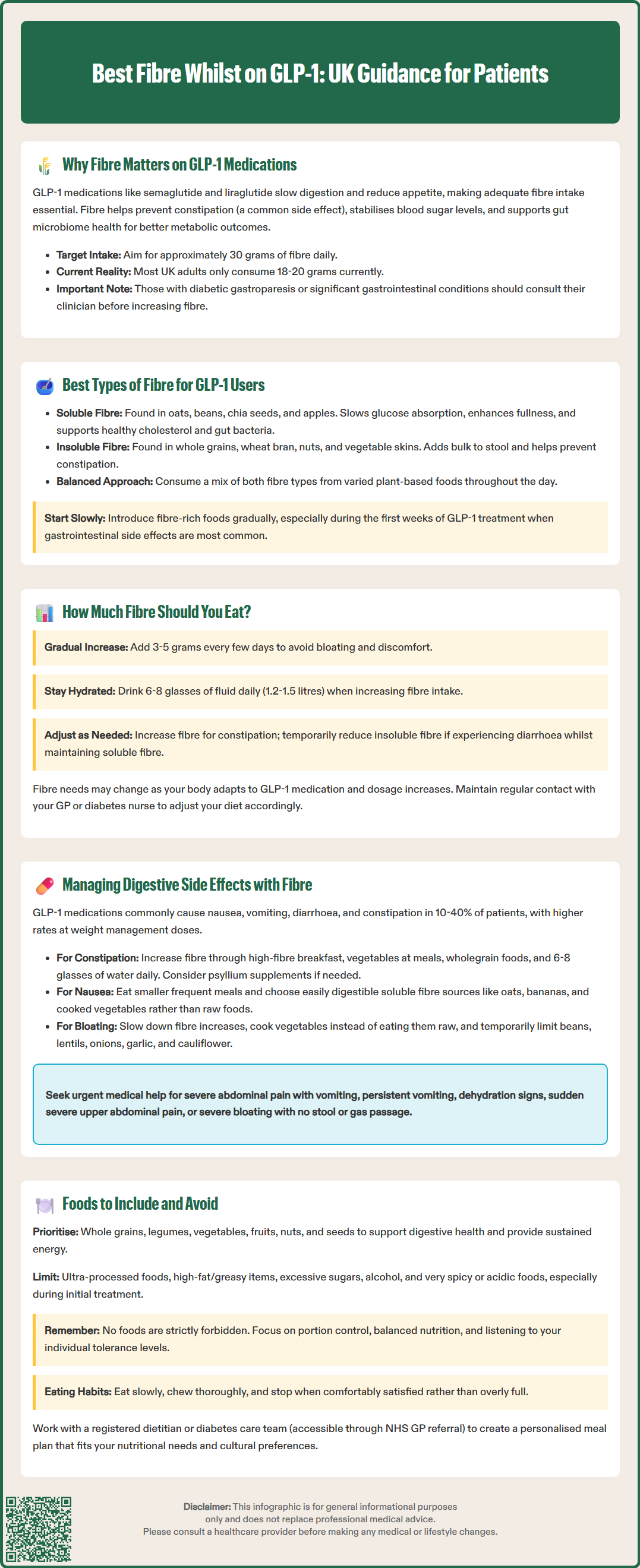
Fibre plays a valuable role in maintaining gastrointestinal health whilst taking GLP-1 medications. As these drugs already slow the movement of food through the digestive system, appropriate fibre intake can help prevent constipation—one of the commonly reported adverse effects. NICE recommends lifestyle and dietary support alongside GLP-1 treatment (NICE NG28), with patients benefiting from comprehensive dietary counselling to optimise treatment outcomes and minimise side effects.
Beyond supporting regular bowel function, fibre offers additional benefits that complement GLP-1 therapy. Soluble fibre helps stabilise blood glucose levels by slowing carbohydrate absorption, which is particularly beneficial for patients with type 2 diabetes. Insoluble fibre promotes regular bowel movements and supports the gut microbiome, which may influence metabolic health and weight management outcomes.
Patients initiating GLP-1 treatment should work with their healthcare team to develop a personalised nutrition plan that incorporates appropriate fibre sources. This proactive approach can improve treatment tolerability and support long-term adherence to these medications. The NHS recommends that adults consume approximately 30 grams of fibre daily, though individual requirements may vary based on treatment response and existing digestive health.
Importantly, people with diabetic gastroparesis or significant gastrointestinal conditions should seek advice from their clinician or dietitian before substantially increasing fibre intake, as high-fibre foods may worsen symptoms in these cases.
Understanding the different types of dietary fibre is essential for patients taking GLP-1 medications, as each type offers distinct benefits and may affect digestive symptoms differently. Dietary fibre is broadly classified into two categories: soluble fibre and insoluble fibre, both of which play complementary roles in supporting gastrointestinal health during GLP-1 therapy.
Soluble fibre dissolves in water to form a gel-like substance in the digestive tract. This type of fibre is particularly beneficial for GLP-1 users because it:
Slows glucose absorption, helping to maintain stable blood sugar levels
Promotes feelings of fullness, which works synergistically with the appetite-suppressing effects of GLP-1 medications
Supports healthy cholesterol levels by binding to bile acids
Feeds beneficial gut bacteria, promoting a healthy microbiome
Excellent sources of soluble fibre include oats, barley, psyllium husk, chia seeds, flaxseeds, beans, lentils, apples, and citrus fruits. These foods are generally well-tolerated by GLP-1 users and can be introduced gradually to minimise digestive discomfort.
Insoluble fibre does not dissolve in water and adds bulk to stool, promoting regular bowel movements—a critical function given the constipation risk associated with GLP-1 therapy. This type of fibre is found in whole grains, wheat bran, nuts, seeds, and the skins of fruits and vegetables.
For optimal results, patients should aim to consume a balanced mixture of both fibre types. A practical approach is to include a variety of plant-based foods throughout the day rather than relying on a single fibre source. For weight management goals, be mindful of portion sizes with energy-dense foods like nuts and seeds (a small handful is typically appropriate).
Some patients may benefit from a gradual introduction of fibre-rich foods, particularly during the initial weeks of GLP-1 treatment when gastrointestinal side effects are most pronounced. If dietary sources prove insufficient, healthcare professionals may recommend fibre supplements such as psyllium or methylcellulose, though these should be introduced under medical supervision. When using fibre supplements, take them with plenty of water and separate them from other oral medicines by at least 2 hours to avoid potential interference with medication absorption.
The NHS recommends that adults consume approximately 30 grams of fibre daily as part of a healthy, balanced diet. This general guidance remains applicable for patients taking GLP-1 medications; however, individual requirements may vary based on treatment response, existing digestive health, and the presence of gastrointestinal side effects.
When initiating GLP-1 therapy, patients should assess their current fibre intake before making significant dietary changes. Many UK adults consume only 18–20 grams of fibre daily, well below the recommended amount. For those starting from a low baseline, a gradual increase is advisable to prevent bloating, gas, and abdominal discomfort. A practical approach is to add 3-5 grams of fibre every few days whilst monitoring digestive tolerance.
Patients experiencing constipation—a side effect reported in clinical trials of GLP-1 agonists (though rates vary by product and dose)—may benefit from gradually working towards the recommended 30 grams daily, ensuring adequate fluid intake alongside. Conversely, those experiencing diarrhoea or loose stools may need to temporarily moderate insoluble fibre intake whilst maintaining adequate soluble fibre to support gut health.
Adequate hydration is essential when increasing fibre consumption, particularly on GLP-1 medications. The NHS recommends 6–8 glasses of fluid daily (approximately 1.2–1.5 litres), with higher amounts during hot weather or increased physical activity. Fibre requires fluid to function effectively in the digestive system, and insufficient fluid intake can paradoxically worsen constipation despite adequate fibre consumption.
It is important to note that fibre requirements may change throughout the course of GLP-1 treatment. As the body adapts to the medication and dosage is titrated upwards, digestive symptoms often evolve. Patients should maintain regular contact with their GP or diabetes specialist nurse to adjust dietary recommendations accordingly. Those with pre-existing gastrointestinal conditions, such as irritable bowel syndrome or inflammatory bowel disease, should receive individualised guidance from a registered dietitian, as standard fibre recommendations may require modification (for example, emphasising soluble fibre or considering a dietitian-supervised low FODMAP approach).
Gastrointestinal adverse effects are among the most commonly reported challenges with GLP-1 medications, with frequency varying by product, dose and indication. According to UK SmPCs, nausea, vomiting, diarrhoea and constipation can affect between 10-40% of patients, with higher rates typically seen at weight management doses. Strategic use of dietary fibre can help mitigate these symptoms and improve treatment tolerability, though the approach must be tailored to the specific digestive complaint.
For constipation, increasing both soluble and insoluble fibre intake is typically beneficial. A practical strategy includes:
Starting the day with a high-fibre breakfast, such as porridge with berries and ground flaxseed
Including vegetables with both lunch and dinner
Choosing wholegrain varieties of bread, pasta, and rice
Ensuring adequate fluid intake (6-8 glasses daily)
Considering a psyllium supplement if dietary measures prove insufficient (taken with plenty of water and separated from other oral medicines by at least 2 hours)
Patients should contact their GP if constipation persists despite these measures, as additional interventions may be required.
For nausea and early satiety, which are particularly common during dose escalation, the approach differs. Whilst maintaining adequate fibre intake remains important, patients may find smaller, more frequent meals easier to tolerate. Soluble fibre sources such as oats, bananas, and well-cooked vegetables are generally better tolerated than raw, high-insoluble-fibre foods during symptomatic periods.
For bloating and gas, which can occur when fibre intake is increased too rapidly, a temporary reduction followed by slower reintroduction is advisable. Cooked vegetables are typically better tolerated than raw ones, and peeling fruits may reduce symptoms. Fermentable fibres found in beans, lentils, and certain vegetables (onions, garlic, cauliflower) may need to be limited initially, then gradually reintroduced as tolerance improves.
Seek urgent medical advice (contact your GP or NHS 111) if you experience:
Severe or persistent abdominal pain, especially if accompanied by vomiting
Persistent vomiting or inability to keep fluids down
Signs of dehydration (extreme thirst, dark urine, dizziness)
Sudden severe upper abdominal pain radiating to the back (possible pancreatitis)
Severe right upper abdominal pain (possible gallstones)
Severe bloating with vomiting and no passage of stool or gas (possible obstruction)
Persistent or severe gastrointestinal symptoms may indicate the need for dose adjustment or, rarely, discontinuation of therapy. Patients are encouraged to report suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Optimising dietary choices whilst taking GLP-1 medications involves both incorporating beneficial high-fibre foods and being mindful of items that may exacerbate digestive symptoms or interfere with treatment goals.
Foods to prioritise for their fibre content and overall nutritional value include:
Whole grains: Oats, barley, quinoa, brown rice, wholemeal bread, and whole-wheat pasta provide sustained energy and both types of fibre
Legumes: Lentils, chickpeas, black beans, and kidney beans offer protein alongside substantial fibre content
Vegetables: Broccoli, Brussels sprouts, carrots, sweet potatoes, and leafy greens supply vitamins, minerals, and fibre
Fruits: Berries, apples (with skin), pears, oranges, and kiwi fruit provide soluble fibre and antioxidants
Seeds and nuts: Chia seeds, flaxseeds, almonds, and walnuts offer healthy fats alongside fibre (keep to a small handful for portion control)
Psyllium husk: A concentrated fibre supplement that can be added to smoothies or yoghurt (take with plenty of water and separate from other oral medicines by at least 2 hours)
Foods to limit or avoid, particularly during the initial treatment phase or when experiencing digestive symptoms:
Ultra-processed foods: These typically contain minimal fibre and may worsen blood glucose control
High-fat, greasy foods: These can exacerbate nausea and slow digestion further, compounding GLP-1 effects
Excessive simple sugars: Sweets, sugary drinks, and refined carbohydrates offer no fibre and may cause blood glucose fluctuations
Alcohol: This can increase nausea risk and provides empty calories that may undermine weight management goals. Those also using insulin or sulfonylureas should be aware of increased hypoglycaemia risk with alcohol
Very spicy or acidic foods: These may aggravate nausea in sensitive individuals
It is important to emphasise that there is no official list of 'forbidden' foods for GLP-1 users. Rather, the focus should be on portion control, balanced nutrition, and individual tolerance. Some patients find that eating slowly, chewing thoroughly, and stopping when comfortably satisfied (rather than full) significantly improves their experience on these medications.
Patients should work with a registered dietitian or their diabetes care team to develop a personalised meal plan that meets their nutritional needs, supports their treatment goals, and accommodates their food preferences and cultural dietary practices. The NHS provides access to dietetic services for patients with diabetes or those prescribed weight management medications through GP referral to local Diabetes Specialist Nurses or Tier 3 weight management services. This support is particularly valuable if dietary management proves challenging.
The NHS recommends approximately 30 grams of fibre daily for adults, including those on GLP-1 therapy. Increase fibre intake gradually (3–5 grams every few days) to prevent bloating and ensure adequate hydration with 6–8 glasses of fluid daily.
Excellent fibre sources include oats, chia seeds, flaxseeds, beans, lentils, apples, whole grains, vegetables, and nuts. Aim for a balanced mix of soluble fibre (oats, beans) and insoluble fibre (whole grains, vegetable skins) to support digestive health and prevent constipation.
Yes, increasing both soluble and insoluble fibre intake can help prevent and manage constipation, a common side effect of GLP-1 therapy. Ensure adequate fluid intake and consider a psyllium supplement if dietary measures prove insufficient, taken with plenty of water and separated from other medicines by at least 2 hours.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.