
Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes treatment. Whilst it does not directly cause vitamin deficiencies, its effects on appetite and gastric emptying can lead to reduced food intake and potentially lower consumption of essential nutrients. Understanding which vitamins to take whilst on Ozempic—and when supplementation may be appropriate—is important for maintaining nutritional adequacy during treatment. This article examines the relationship between Ozempic and vitamin levels, identifies key nutrients to monitor, and provides guidance on when to seek professional advice regarding supplementation.
Quick Answer: Ozempic does not directly cause vitamin deficiencies, but reduced appetite may lower intake of essential nutrients including B vitamins, vitamin D, and calcium.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
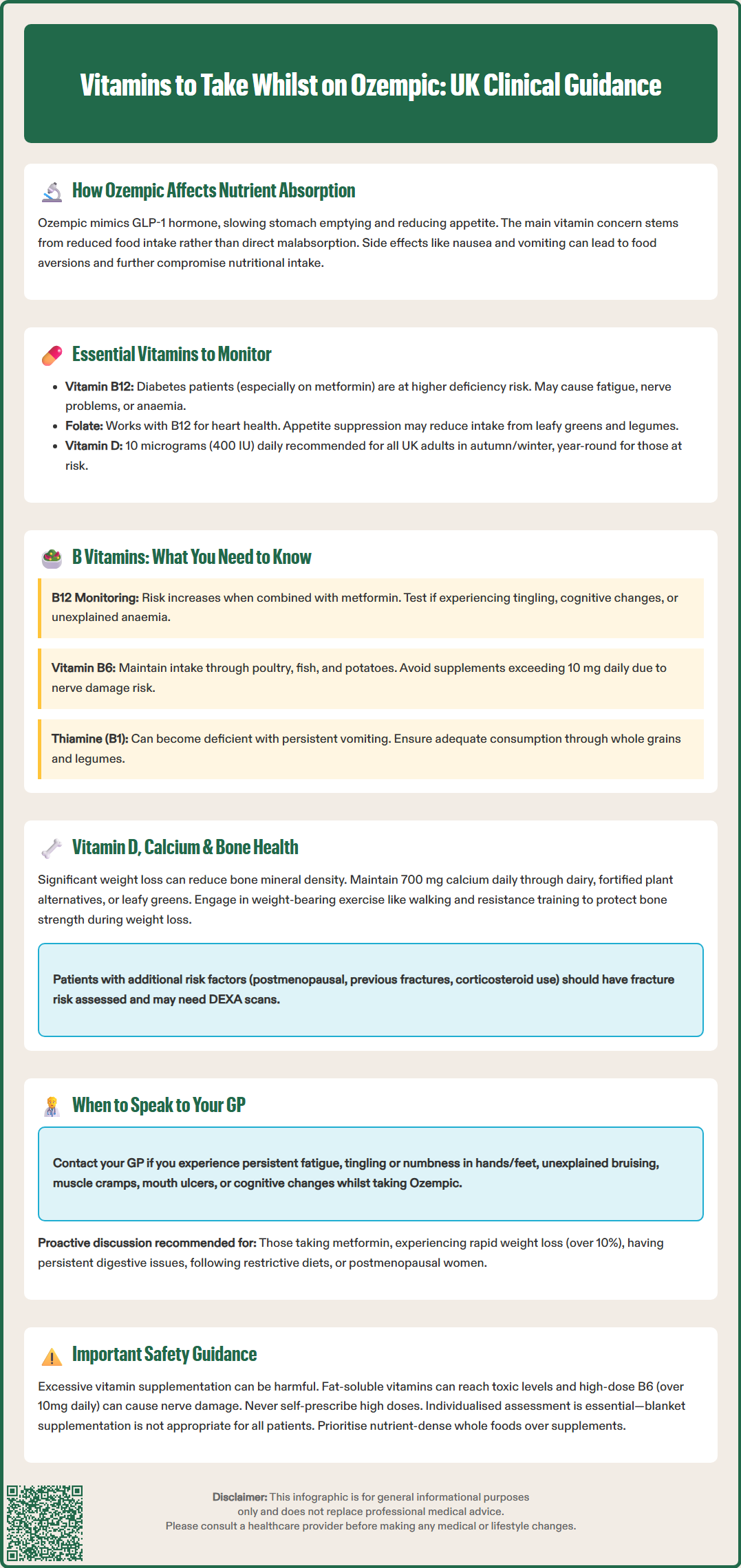
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It works by mimicking the action of the naturally occurring hormone GLP-1, which slows gastric emptying, reduces appetite, and enhances insulin secretion in response to meals. Whilst these mechanisms contribute to improved glycaemic control and often significant weight loss, the delayed gastric emptying can have implications for dietary intake.
The primary concern regarding vitamin levels in patients taking Ozempic relates to reduced food intake rather than direct malabsorption. Many individuals experience decreased appetite and early satiety, leading to smaller portion sizes and potentially less diverse diets. This reduction in overall caloric intake may inadvertently result in lower consumption of essential vitamins and minerals, particularly if dietary quality is not maintained.
Additionally, gastrointestinal adverse effects—including nausea (very common), vomiting, and diarrhoea—can further compromise nutritional status. These symptoms, which are most common during dose escalation, may lead to food aversions or avoidance of certain nutrient-dense foods. It's important to note that the delayed gastric emptying effect tends to be transient and the Ozempic Summary of Product Characteristics (SmPC) reports no clinically relevant effect on the absorption of most oral medicines or nutrients.
It is important to emphasise that current evidence does not demonstrate that Ozempic directly causes vitamin deficiencies or malabsorption. However, the indirect effects on dietary intake and gastrointestinal function warrant attention to nutritional adequacy, particularly in patients experiencing substantial weight loss or prolonged gastrointestinal symptoms.
Note: Wegovy (semaglutide) is the brand name licensed specifically for weight management in the UK, while Ozempic is licensed for type 2 diabetes treatment.
Maintaining adequate vitamin intake whilst taking Ozempic requires a proactive approach to nutrition, particularly for individuals experiencing significant weight loss or reduced dietary variety. The most commonly discussed vitamins in this context include the B-complex vitamins, vitamin D, and certain minerals such as calcium and magnesium, though comprehensive nutritional assessment should be individualised.
Vitamin B12 (cobalamin) deserves particular attention, as patients with type 2 diabetes—especially those taking metformin concurrently—are already at increased risk of deficiency. Vitamin B12 is essential for neurological function, red blood cell formation, and DNA synthesis. Deficiency can manifest as fatigue, peripheral neuropathy, or macrocytic anaemia. Whilst there is no direct mechanism by which semaglutide depletes B12, reduced intake of animal products (a primary dietary source) during weight loss may contribute to suboptimal levels.
Folate (vitamin B9) works synergistically with B12 in cellular metabolism and is particularly important for cardiovascular health. Adequate folate intake supports homocysteine metabolism, which is relevant given the cardiovascular risk profile of many patients with type 2 diabetes. Good dietary sources include leafy green vegetables, fortified cereals, and legumes—foods that may be consumed in smaller quantities during appetite suppression.
Vitamin C (ascorbic acid) supports immune function, collagen synthesis, and iron absorption. Patients experiencing food aversions or limited fruit and vegetable intake may benefit from ensuring adequate vitamin C consumption through dietary modification or supplementation.
Vitamin D is recommended by the NHS at 10 micrograms (400 IU) daily for all adults during autumn and winter months (October to March), and year-round for people at risk of deficiency. The UK reference nutrient intake for calcium is 700 mg daily for adults, according to NHS guidance.
A balanced, nutrient-dense diet remains the cornerstone of vitamin adequacy. Patients should be encouraged to prioritise quality over quantity, focusing on whole foods, lean proteins, colourful vegetables, and whole grains within their reduced caloric intake. High-dose supplementation of antioxidants or vitamins is not routinely recommended without evidence of deficiency.
The B-vitamin complex comprises eight distinct vitamins (B1, B2, B3, B5, B6, B7, B9, and B12), each with specific roles in energy metabolism, nervous system function, and cellular health. For patients taking Ozempic, particular attention should be paid to vitamin B12, B6, and folate, given their importance in neurological health and their potential vulnerability during dietary restriction.
Vitamin B12 deficiency is relatively common in patients with type 2 diabetes, particularly among those taking metformin. Metformin can interfere with B12 absorption in the terminal ileum, and this effect may increase with duration of therapy. When Ozempic is added to existing metformin therapy, the combined impact of reduced dietary intake and potential impaired absorption warrants consideration. The MHRA Drug Safety Update (2022) and NICE guidance recommend testing B12 levels in patients on metformin who develop symptoms suggestive of deficiency (paraesthesia, glossitis, cognitive changes, or unexplained anaemia) and considering periodic monitoring in those on long-term therapy, particularly with risk factors for deficiency.
Vitamin B6 (pyridoxine) is involved in amino acid metabolism, neurotransmitter synthesis, and haemoglobin formation. Whilst frank deficiency is uncommon in the UK, suboptimal intake may occur with restrictive eating patterns. Dietary sources include poultry, fish, potatoes, and fortified cereals. There is no established link between semaglutide and B6 deficiency, but maintaining adequate intake supports overall metabolic health. The NHS advises against taking more than 10 mg of B6 supplements daily unless under medical supervision, as excessive amounts can lead to peripheral neuropathy.
Thiamine (vitamin B1) deficiency, though rare in the UK, can occur in the context of persistent vomiting or very low carbohydrate intake. Severe deficiency can lead to Wernicke's encephalopathy or beriberi, though these are exceptional circumstances. Patients experiencing prolonged gastrointestinal symptoms should ensure adequate thiamine intake through whole grains, legumes, and fortified foods.
Routine supplementation with a B-complex vitamin may be considered for patients with documented deficiency, those on concurrent metformin with risk factors, or individuals struggling to maintain dietary variety. However, supplementation should be guided by clinical assessment rather than adopted universally.
Bone health is an important consideration for patients undergoing significant weight loss, as substantial reduction in body weight can affect bone mineral density through multiple mechanisms. Vitamin D and calcium are the primary nutrients supporting skeletal integrity, and their adequacy should be monitored in patients taking Ozempic, particularly those losing substantial weight or with pre-existing risk factors for osteoporosis.
Vitamin D is essential for calcium absorption, bone mineralisation, immune function, and muscle strength. In the UK, vitamin D deficiency is common, particularly during autumn and winter months when sunlight exposure is insufficient for cutaneous synthesis. The NHS recommends that all adults consider taking a daily supplement containing 10 micrograms (400 IU) of vitamin D, especially between October and March. For patients taking Ozempic, this recommendation becomes even more pertinent, as reduced dietary intake may limit consumption of vitamin D-rich foods such as oily fish, fortified dairy products, and eggs.
Rapid, substantial weight loss can lead to increased bone turnover and potential reduction in bone mineral density. This occurs because mechanical loading on the skeleton decreases, and hormonal changes associated with weight loss may affect bone metabolism. Adequate calcium intake (700 mg daily for adults in the UK, according to NHS guidance) helps mitigate this risk. Dairy products, fortified plant-based alternatives, leafy greens, and tinned fish with bones provide dietary calcium.
NICE guidance (NG226) on osteoporosis prevention emphasises the importance of adequate calcium and vitamin D intake, weight-bearing exercise, and smoking cessation. Patients taking Ozempic who have additional risk factors—such as postmenopausal status, previous fragility fractures, long-term corticosteroid use, or family history of osteoporosis—should have their fracture risk assessed using validated tools such as FRAX or QFracture. Based on this assessment, bone density measurement (DEXA scan) and more intensive monitoring may be warranted according to NICE pathways.
Patients should be advised to maintain weight-bearing physical activity (walking, resistance training) alongside nutritional optimisation to support bone health during weight loss. If dietary intake of calcium and vitamin D is insufficient, supplementation should be discussed with a healthcare professional.
Whilst maintaining a balanced diet should be the primary strategy for meeting nutritional needs, certain circumstances warrant discussion with your GP or healthcare team regarding vitamin supplementation. Individualised assessment is essential, as blanket supplementation is neither necessary nor appropriate for all patients taking Ozempic.
You should contact your GP if you experience symptoms that may indicate vitamin deficiency, including:
Persistent fatigue or weakness that does not improve with adequate sleep
Neurological symptoms such as tingling, numbness, or burning sensations in hands or feet (peripheral neuropathy)
Unexplained bruising or bleeding (which requires prompt medical assessment for various potential causes)
Muscle cramps, bone pain, or fractures, potentially indicating calcium or vitamin D deficiency
Mouth ulcers, glossitis (inflamed tongue), or angular cheilitis, which may reflect B-vitamin deficiencies
Cognitive changes, memory problems, or mood disturbances that could relate to B12 or folate deficiency
Additionally, certain patient groups should proactively discuss vitamin supplementation with their healthcare provider:
Those taking metformin concurrently, particularly if experiencing symptoms suggestive of B12 deficiency or with risk factors for deficiency
Individuals experiencing rapid or substantial weight loss (more than 10% of body weight)
Patients with persistent gastrointestinal symptoms (nausea, vomiting, diarrhoea lasting beyond the initial titration period)
Those following restrictive dietary patterns (vegetarian, vegan, or elimination diets)
Older adults, particularly postmenopausal women at increased risk of osteoporosis
Your GP can arrange appropriate blood tests to assess vitamin and mineral status, including full blood count, B12, folate, 25-hydroxyvitamin D, calcium, alkaline phosphatase, and other parameters as clinically indicated. Based on these results and your individual circumstances, they can recommend specific supplementation regimens and appropriate doses.
It is important to note that excessive supplementation can be harmful—fat-soluble vitamins (A, D, E, K) can accumulate to toxic levels, and high-dose B6 (over 10 mg daily) can cause neuropathy. Always seek professional guidance rather than self-prescribing high-dose supplements.
If you experience any suspected side effects from Ozempic, report them via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Ozempic does not directly cause vitamin deficiencies or malabsorption. However, reduced appetite and food intake may lead to lower consumption of essential vitamins and minerals, particularly if dietary quality is not maintained during treatment.
Vitamin B12 supplementation may be appropriate if you are taking metformin concurrently, have documented deficiency, or experience symptoms such as fatigue or peripheral neuropathy. Discuss blood testing and supplementation with your GP rather than self-prescribing.
Contact your GP if you experience symptoms of deficiency (persistent fatigue, neurological symptoms, muscle cramps), are losing substantial weight, have persistent gastrointestinal symptoms, take metformin concurrently, or follow restrictive dietary patterns. Your GP can arrange appropriate blood tests and recommend individualised supplementation.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.