
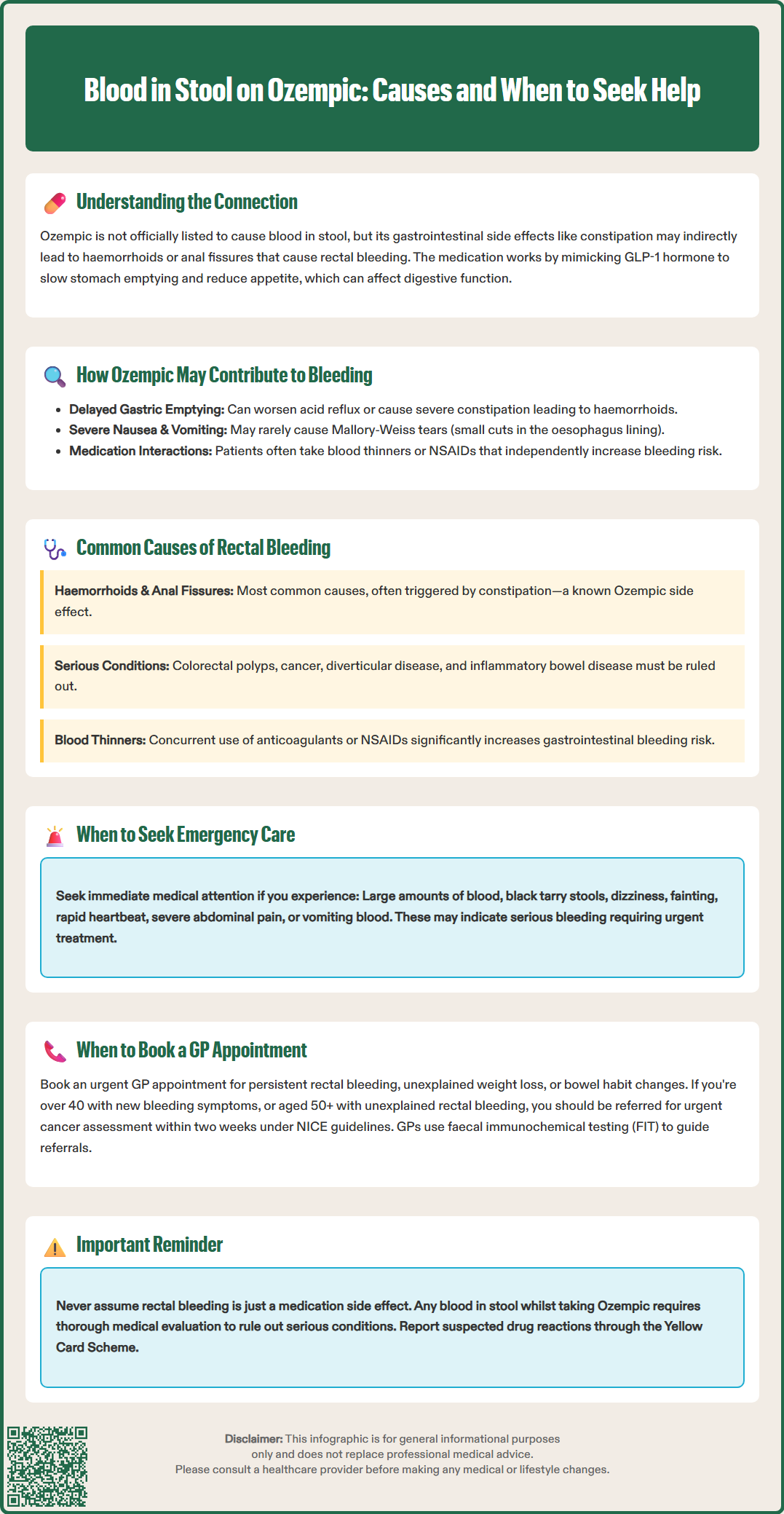
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for type 2 diabetes mellitus and weight management. Whilst blood in stool is not a recognised adverse reaction in the MHRA-approved Summary of Product Characteristics, patients may experience gastrointestinal side effects—such as constipation—that can indirectly contribute to rectal bleeding. This article examines the relationship between Ozempic and rectal bleeding, outlines when urgent medical attention is required, and explores alternative causes of this symptom in patients prescribed semaglutide.
Quick Answer: Blood in stool is not a recognised adverse reaction to Ozempic, but the medication's gastrointestinal side effects may indirectly contribute to conditions causing rectal bleeding.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus and, at higher doses (as Wegovy), for weight management in adults with obesity. The medication works by mimicking the action of the naturally occurring hormone GLP-1, which stimulates insulin secretion, suppresses glucagon release, slows gastric emptying, and reduces appetite.
Whilst Ozempic has demonstrated significant efficacy in glycaemic control and weight reduction, it is associated with a range of gastrointestinal adverse effects. According to the MHRA-approved Summary of Product Characteristics (SmPC), the most commonly reported side effects include nausea, vomiting, diarrhoea, abdominal pain, and constipation. These effects are typically mild to moderate in severity and often diminish over time as the body adjusts to the medication.
Blood in the stool (rectal bleeding or haematochezia) is not listed as an adverse reaction in the MHRA/EMC SmPC for Ozempic or Wegovy. However, patients taking Ozempic may experience gastrointestinal symptoms that could indirectly contribute to conditions associated with rectal bleeding, such as constipation leading to haemorrhoids or anal fissures. It is essential to recognise that the presence of blood in stool whilst taking Ozempic warrants thorough clinical evaluation, as multiple potential causes exist—some potentially related to the medication's gastrointestinal effects and others entirely independent of semaglutide therapy.
This article provides evidence-based guidance on the relationship between Ozempic and rectal bleeding, when to seek urgent medical attention, and alternative explanations for this symptom in patients prescribed this medication.
Gastrointestinal bleeding is not a recognised adverse reaction in the MHRA-approved SmPC for Ozempic, and current evidence from clinical trials has not identified an increased risk. The extensive SUSTAIN and STEP clinical trial programmes, which evaluated semaglutide's safety and efficacy, have not shown a signal for increased incidence of gastrointestinal bleeding compared to placebo or active comparators, as documented in the European Medicines Agency's European Public Assessment Report (EPAR).
However, Ozempic's mechanism of action—particularly delayed gastric emptying—can exacerbate certain pre-existing gastrointestinal conditions. The slowing of gastric motility may worsen gastro-oesophageal reflux disease (GORD) or contribute to constipation, both of which can indirectly lead to complications associated with bleeding. Severe or chronic constipation, for instance, may result in anal fissures or haemorrhoids, which are common benign causes of bright red rectal bleeding.
Additionally, the nausea and vomiting associated with Ozempic can, in rare instances, be severe. While not a listed adverse reaction in the SmPC, persistent forceful vomiting can theoretically lead to Mallory-Weiss tears—small lacerations in the oesophageal mucosa that may bleed. Such cases would be uncommon, and persistent or forceful vomiting should be reported to a healthcare professional promptly.
It is also important to consider that patients prescribed Ozempic for type 2 diabetes may have other risk factors for gastrointestinal pathology, including concurrent use of antiplatelet agents (such as aspirin) or anticoagulants, which independently increase bleeding risk. Non-steroidal anti-inflammatory drugs (NSAIDs), commonly used for pain relief, are well-established causes of gastric and duodenal ulceration and should be used cautiously in this population.
Any episode of rectal bleeding warrants clinical assessment, particularly in individuals over 50 years of age or those with additional risk factors for colorectal pathology. The urgency of evaluation depends on the volume of blood, associated symptoms, and the patient's overall clinical condition.
Seek immediate medical attention (attend A&E or call 999) if you experience:
Large volumes of blood in the stool or blood clots
Melaena—black, tarry, foul-smelling stools suggesting upper gastrointestinal bleeding
Dizziness, light-headedness, or fainting, which may indicate significant blood loss and haemodynamic compromise
Rapid heart rate, pallor, or shortness of breath—signs of anaemia or shock
Severe, persistent abdominal pain or distension
Vomiting blood (haematemesis) or coffee-ground material
Arrange an urgent GP appointment if:
You notice persistent or recurrent small amounts of bright red blood on toilet paper or mixed with stool
You have unexplained weight loss, change in bowel habit, or persistent abdominal discomfort
You are aged over 40 years and experiencing new-onset rectal bleeding
You have a family history of colorectal cancer or inflammatory bowel disease
According to NICE guidance (NG12), patients should be referred on an urgent suspected cancer pathway (within two weeks) in several scenarios, including: adults aged 50 and over with unexplained rectal bleeding; those aged 40 and over with unexplained weight loss and abdominal pain; those aged 60 and over with iron-deficiency anaemia or change in bowel habit; and anyone with a rectal or abdominal mass.
In primary care, faecal immunochemical testing (FIT) is now used to guide referral decisions. A result of ≥10 µg Hb/g faeces should prompt urgent suspected cancer referral. However, if a rectal mass or anal ulceration is present, patients should be referred directly without FIT testing.
Do not assume that rectal bleeding is simply a side effect of Ozempic. Prompt evaluation ensures that serious underlying conditions, including colorectal malignancy, inflammatory bowel disease, or significant gastrointestinal bleeding, are not missed. If symptoms persist or worsen, seek further medical advice even if initial investigations are reassuring.
Whilst taking Ozempic, several alternative explanations for rectal bleeding should be considered, many of which are more common than any potential drug-related effect.
Haemorrhoids (piles) are the most frequent cause of bright red rectal bleeding in adults. These swollen blood vessels in the anal canal may develop or worsen due to constipation—a recognised side effect of Ozempic. Straining during bowel movements increases intra-abdominal pressure, predisposing to haemorrhoidal bleeding. Patients may notice blood on toilet paper, in the toilet bowl, or coating the stool.
Anal fissures—small tears in the anal lining—also commonly result from constipation or passing hard stools. These typically cause sharp pain during and after defecation, accompanied by small amounts of bright red blood. Both haemorrhoids and fissures are generally benign and respond well to conservative management, including increased dietary fibre, adequate hydration, and topical treatments.
Diverticular disease is another important consideration, particularly in older adults. Diverticula are small pouches that form in the colonic wall and may bleed, sometimes profusely, without prior symptoms. Diverticular bleeding is typically painless and may present as maroon or bright red blood.
Inflammatory bowel disease (IBD), including Crohn's disease and ulcerative colitis, can cause rectal bleeding accompanied by diarrhoea, abdominal pain, and systemic symptoms such as weight loss and fatigue. Whilst IBD is not caused by Ozempic, patients with undiagnosed IBD may coincidentally be prescribed the medication.
Infectious or ischaemic colitis can also present with rectal bleeding, particularly in older adults or those with vascular risk factors. These conditions typically cause abdominal pain and diarrhoea alongside bleeding.
Colorectal polyps and cancer must always be excluded, particularly in patients over 50 or those with alarm features. Polyps are often asymptomatic but may bleed intermittently. Colorectal cancer may present with rectal bleeding, altered bowel habit, unexplained anaemia, or abdominal mass.
Medication-related causes should also be reviewed. Concurrent use of anticoagulants (warfarin, DOACs), antiplatelet agents (aspirin, clopidogrel), or NSAIDs significantly increases the risk of gastrointestinal bleeding. If bleeding occurs, NSAIDs should be avoided, and anticoagulant/antiplatelet therapy should be reviewed with a healthcare professional. Patients taking these medications alongside Ozempic require careful monitoring and should report any bleeding promptly.
Gastric or duodenal ulceration may occur, particularly in patients taking NSAIDs or with Helicobacter pylori infection. Upper gastrointestinal bleeding typically presents as melaena rather than bright red rectal bleeding, though brisk upper GI bleeding can occasionally present as haematochezia.
In conclusion, whilst blood in the stool may occur during Ozempic therapy, it is essential to investigate thoroughly to identify the underlying cause. Patients should maintain open communication with their healthcare team and not delay seeking medical advice when rectal bleeding occurs. If you suspect an adverse reaction to Ozempic, report it to the MHRA through the Yellow Card Scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Blood in stool is not a recognised adverse reaction in the MHRA-approved Summary of Product Characteristics for Ozempic. However, gastrointestinal side effects such as constipation may indirectly contribute to conditions like haemorrhoids or anal fissures that cause rectal bleeding.
Seek immediate medical attention if you experience large volumes of blood, black tarry stools (melaena), dizziness, rapid heart rate, severe abdominal pain, or vomiting blood. Arrange an urgent GP appointment for persistent small amounts of blood, unexplained weight loss, or if you are over 40 with new-onset rectal bleeding.
The most common causes include haemorrhoids and anal fissures, often related to constipation. Other possibilities include diverticular disease, inflammatory bowel disease, colorectal polyps or cancer, and medication-related bleeding from concurrent use of anticoagulants, antiplatelet agents, or NSAIDs.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.