Can I take weight loss injections with methotrexate? Many patients prescribed methotrexate for rheumatoid arthritis, psoriasis, or other inflammatory conditions also seek weight management support. Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly available in the UK. Whilst there is no specific contraindication to combining these medications, and no direct drug interaction has been identified, several important safety considerations require careful evaluation. This article examines the evidence, potential risks, and essential discussions needed with your healthcare provider before considering this combination therapy.
Quick Answer: There is no specific contraindication to taking weight loss injections (GLP-1 receptor agonists) with methotrexate, and no direct drug interaction has been identified between these medication classes.
Methotrexate is a disease-modifying antirheumatic drug (DMARD) commonly prescribed in the UK for conditions such as rheumatoid arthritis, psoriasis, psoriatic arthritis, and certain inflammatory bowel diseases. It works by inhibiting dihydrofolate reductase and, at lower doses used in rheumatology, through adenosine-mediated anti-inflammatory effects. This helps reduce inflammation and slow disease progression. In rheumatology, methotrexate is typically administered once weekly at doses ranging from 7.5mg to 25mg, either orally or by subcutaneous injection.
Methotrexate affects rapidly dividing cells throughout the body, which means it can interact with numerous medications. The drug is primarily eliminated by the kidneys with limited hepatic metabolism, making renal function particularly important for safe use. Impaired kidney function or dehydration can significantly increase the risk of toxicity. Common adverse effects include nausea, mouth ulcers, fatigue, and increased susceptibility to infections due to bone marrow suppression.
Key drug interactions with methotrexate include:
Non-steroidal anti-inflammatory drugs (NSAIDs) may increase methotrexate levels, though many can be used with caution at low-dose methotrexate with appropriate monitoring
Trimethoprim and co-trimoxazole are contraindicated due to increased folate antagonism
Proton pump inhibitors may affect methotrexate levels, particularly with high-dose methotrexate regimens
Certain antibiotics, particularly penicillins, that can reduce renal clearance
Patients taking methotrexate require regular blood monitoring, including full blood count, liver function, and renal function. Monitoring is typically more frequent initially (every 1-2 weeks), then every 2-3 months once stable. The MHRA has issued specific guidance emphasising the importance of once-weekly dosing to prevent potentially fatal overdose errors. Patients should also be advised to avoid or limit alcohol consumption due to increased risk of hepatotoxicity.
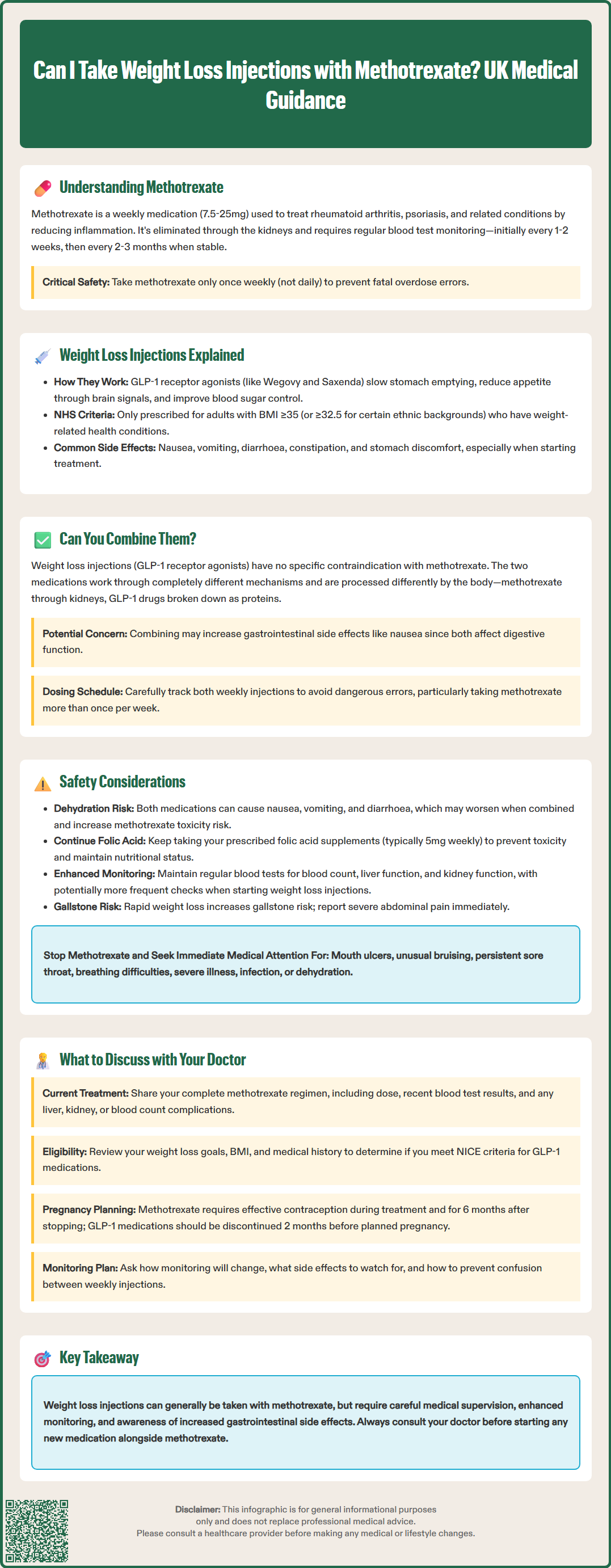
Weight loss injections have gained considerable attention in recent years, with several types now available through NHS prescription or private healthcare in the UK. The most commonly discussed medications belong to the glucagon-like peptide-1 (GLP-1) receptor agonist class, including semaglutide (marketed as Wegovy for weight management or Ozempic for type 2 diabetes) and liraglutide (Saxenda for weight management or Victoza for diabetes).
These medications work by mimicking the action of GLP-1, a naturally occurring hormone that regulates appetite and blood sugar levels. GLP-1 receptor agonists achieve weight loss through several mechanisms:
Slowing gastric emptying, which promotes feelings of fullness
Reducing appetite by acting on brain centres that control hunger
Improving insulin secretion and reducing glucagon release
Potentially affecting food reward pathways in the brain
According to NICE Technology Appraisal guidance (TA875 for semaglutide/Wegovy and TA664 for liraglutide/Saxenda), these medications may be considered for weight management in adults with a BMI of at least 35 kg/m² (or 32.5 kg/m² for people from South Asian, Chinese, other Asian, Middle Eastern, Black African, or African-Caribbean family backgrounds) with at least one weight-related comorbidity. They are only available through specialist weight management services after lifestyle interventions have been unsuccessful.
Common side effects include nausea, vomiting, diarrhoea, constipation, and abdominal discomfort, particularly during the initial titration phase. More serious but rare adverse effects include pancreatitis and gallbladder disease. Preclinical studies have identified thyroid C-cell tumours in rodents, so patients should report any symptoms such as neck mass, hoarseness, or difficulty swallowing. For people with diabetes, there is also a risk of diabetic retinopathy progression, particularly with rapid improvement in blood glucose control.
It's important to note that there are currently supply constraints for GLP-1 receptor agonists in the UK, and NHS England advises against using Ozempic off-label for weight management to ensure availability for diabetes patients.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereThe question of whether weight loss injections can be safely combined with methotrexate is increasingly relevant, as many patients with inflammatory conditions managed by methotrexate also struggle with weight management. This may be due to reduced mobility from joint disease, corticosteroid use, or metabolic changes associated with chronic inflammation. According to the Summary of Product Characteristics (SmPC) for both methotrexate and GLP-1 receptor agonists, there is no specific contraindication to using these medications together, and no direct pharmacological interaction has been identified between these medication classes.
GLP-1 receptor agonists are not known to significantly affect the renal elimination or limited hepatic metabolism of methotrexate, nor do they interfere with folate metabolism—the primary pathway through which methotrexate exerts its therapeutic and toxic effects. From a pharmacokinetic perspective, these medications work through entirely different mechanisms and are processed differently by the body. Methotrexate primarily undergoes renal excretion, whilst GLP-1 analogues are broken down through protein degradation pathways.
However, the absence of a direct drug-drug interaction does not automatically mean the combination is without considerations. Both medication classes can affect gastrointestinal function, and combining them may potentially amplify certain side effects, particularly nausea and gastrointestinal upset. Additionally, the delayed gastric emptying caused by GLP-1 receptor agonists could theoretically affect the absorption of oral methotrexate, though this remains largely theoretical and has not been well-studied. This concern is less relevant for patients using subcutaneous methotrexate injections.
A practical safety consideration is the risk of dosing confusion when both medications are administered weekly. Methotrexate must never be taken more than once weekly, and adding another weekly injection (such as semaglutide/Wegovy) requires careful scheduling and reminder systems to prevent potentially serious dosing errors.
When considering weight loss injections alongside methotrexate, several safety considerations warrant careful attention. Whilst there is no direct pharmacological interaction documented in the SmPCs, the combination may present indirect risks that require monitoring and management.
Gastrointestinal effects represent the most common concern. Both methotrexate and GLP-1 receptor agonists can cause nausea, vomiting, and diarrhoea. According to product information, methotrexate-induced nausea affects a significant proportion of patients, whilst GLP-1 agonists frequently cause gastrointestinal side effects, particularly during dose escalation. When combined, these effects may be additive, potentially leading to reduced medication adherence or increased discomfort. Severe gastrointestinal symptoms could also lead to dehydration, which may increase the risk of methotrexate toxicity by affecting renal function.
Nutritional status is another important consideration. Methotrexate therapy requires adequate folate supplementation (typically 5mg once weekly, taken on a different day from methotrexate) to reduce toxicity. Significant weight loss and reduced food intake associated with GLP-1 agonists could potentially affect overall nutritional status. Patients should be advised to maintain adequate nutrition and continue their prescribed folic acid supplementation without interruption.
Monitoring requirements become particularly important with combination therapy. Patients on methotrexate already require regular blood tests to monitor full blood count, liver function, and renal function. These monitoring schedules should be maintained and potentially intensified when starting weight loss injections, particularly if gastrointestinal side effects are significant. Any signs of methotrexate toxicity—including mouth ulcers, unusual bruising, persistent sore throat, or shortness of breath—require immediate medical attention.
Additional safety considerations include:
Sick-day rules: Methotrexate should be temporarily withheld during severe illness, infection, or dehydration; consult your healthcare provider if unwell
Gallstone risk: Rapid weight loss increases the risk of gallstones; report severe abdominal pain promptly
Diabetic retinopathy: For people with diabetes, rapid improvement in blood glucose control with GLP-1 agonists may worsen retinopathy
Alcohol: Limit or avoid alcohol consumption while taking methotrexate due to increased risk of liver toxicity
Patients should report suspected side effects to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Before initiating weight loss injections whilst taking methotrexate, a comprehensive discussion with your healthcare provider is essential. This conversation should cover multiple aspects of your health, treatment goals, and potential risks to ensure safe and effective therapy.
Your current methotrexate regimen should be thoroughly reviewed, including your dose, duration of treatment, disease control, and any previous adverse effects. Inform your doctor about your most recent blood test results and whether you have experienced any methotrexate-related complications such as liver enzyme elevations, low blood counts, or kidney function changes. If your disease is not well controlled or you have recently had dose adjustments, it may be advisable to achieve stability before adding another medication.
Your weight loss goals and medical history require detailed discussion. Be prepared to discuss your BMI, previous weight loss attempts, any obesity-related comorbidities (such as type 2 diabetes, hypertension, or sleep apnoea), and your realistic expectations for treatment. Your doctor will need to assess whether you meet NICE criteria (TA875 for semaglutide/Wegovy or TA664 for liraglutide/Saxenda) and whether referral to a specialist weight management service is appropriate.
Pregnancy and contraception planning is crucial to discuss. Methotrexate is teratogenic (harmful to a developing foetus) and must be avoided during pregnancy and breastfeeding. Effective contraception is essential during treatment and for at least 6 months after stopping methotrexate. GLP-1 receptor agonists are also not recommended during pregnancy and should be discontinued at least 2 months before a planned pregnancy (for semaglutide).
Key questions to ask your healthcare provider include:
Are there any specific concerns about combining these medications given my individual health status?
How will my monitoring schedule change if I start weight loss injections?
What side effects should I watch for, and when should I seek urgent medical attention?
How can I prevent confusion between weekly methotrexate and weekly GLP-1 injections (if applicable)?
Should I adjust the timing of my medications or folic acid supplementation?
What dietary considerations should I follow to maintain adequate nutrition?
What is my vaccination status, and are there any vaccines I should receive or avoid?
How will we assess whether the treatment is working, and what are the criteria for continuing or stopping?
Practical considerations should also be addressed, including current UK supply constraints for GLP-1 medications, NHS access pathways, injection technique training, and storage requirements. Discuss your support network and whether you would benefit from referral to specialist services such as dietetics or rheumatology for coordinated care. Finally, ensure you understand the warning signs that require immediate medical attention, including severe abdominal pain, persistent vomiting, signs of pancreatitis, or any symptoms suggesting methotrexate toxicity.
There is no direct pharmacological interaction between GLP-1 receptor agonists (weight loss injections) and methotrexate documented in UK product information. However, both medications can cause gastrointestinal side effects that may be additive, and careful monitoring is required.
Continue your regular methotrexate blood monitoring schedule (full blood count, liver function, and renal function tests). Your healthcare provider may intensify monitoring when starting weight loss injections, particularly if you experience significant gastrointestinal side effects or dehydration.
NHS access to GLP-1 receptor agonists for weight management follows NICE guidance and requires referral to specialist weight management services after lifestyle interventions have been unsuccessful. Your rheumatology team and weight management service will need to coordinate care to ensure safe prescribing alongside methotrexate.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.