Rybelsus (semaglutide) is an oral GLP-1 receptor agonist licensed in the UK for managing type 2 diabetes mellitus in adults. Whilst patients taking Rybelsus may occasionally develop urinary tract infections (UTIs), current clinical evidence does not establish a direct causal link between the medication and UTIs. People with diabetes are inherently at increased risk of UTIs due to elevated blood glucose levels and diabetes-related complications. Understanding the distinction between Rybelsus's recognised side effects—predominantly gastrointestinal—and unrelated conditions such as UTIs is essential for safe and effective diabetes management. This article examines whether Rybelsus can cause UTIs, reviews the evidence, and provides guidance on recognising and managing urinary symptoms.
Quick Answer: Rybelsus (semaglutide) does not directly cause urinary tract infections based on current clinical evidence and regulatory data.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereRybelsus (semaglutide) is an oral medication licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It is indicated as monotherapy when metformin is inappropriate, or in combination with other glucose-lowering medicines. It belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists. Rybelsus is typically prescribed alongside diet and exercise modifications to improve glycaemic control.
The mechanism of action centres on mimicking the naturally occurring hormone GLP-1, which is released by the gut in response to food intake. Semaglutide binds to GLP-1 receptors on pancreatic beta cells, stimulating insulin secretion in a glucose-dependent manner—meaning insulin is released only when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared with some other diabetes medications. Additionally, Rybelsus suppresses glucagon secretion (a hormone that raises blood glucose), slows gastric emptying, and promotes satiety, which can contribute to weight loss, although it is not licensed for weight management in the UK.
Rybelsus is available in three tablet strengths: 3 mg, 7 mg, and 14 mg. Treatment usually begins with the 3 mg dose for 30 days to allow the body to adjust, before increasing to 7 mg. After at least 30 days on 7 mg, the dose may be increased to 14 mg if additional glycaemic control is needed. The tablets must be taken on an empty stomach with a small amount of water (up to 120 ml), at least 30 minutes before any food, drink, or other oral medications. Tablets should be swallowed whole and not split, crushed or chewed. This specific administration requirement is crucial for optimal absorption, as semaglutide's oral bioavailability is naturally low.
As with all medications, Rybelsus carries a profile of potential side effects. Understanding these—and distinguishing them from unrelated conditions such as urinary tract infections—is important for patient safety and effective diabetes management.
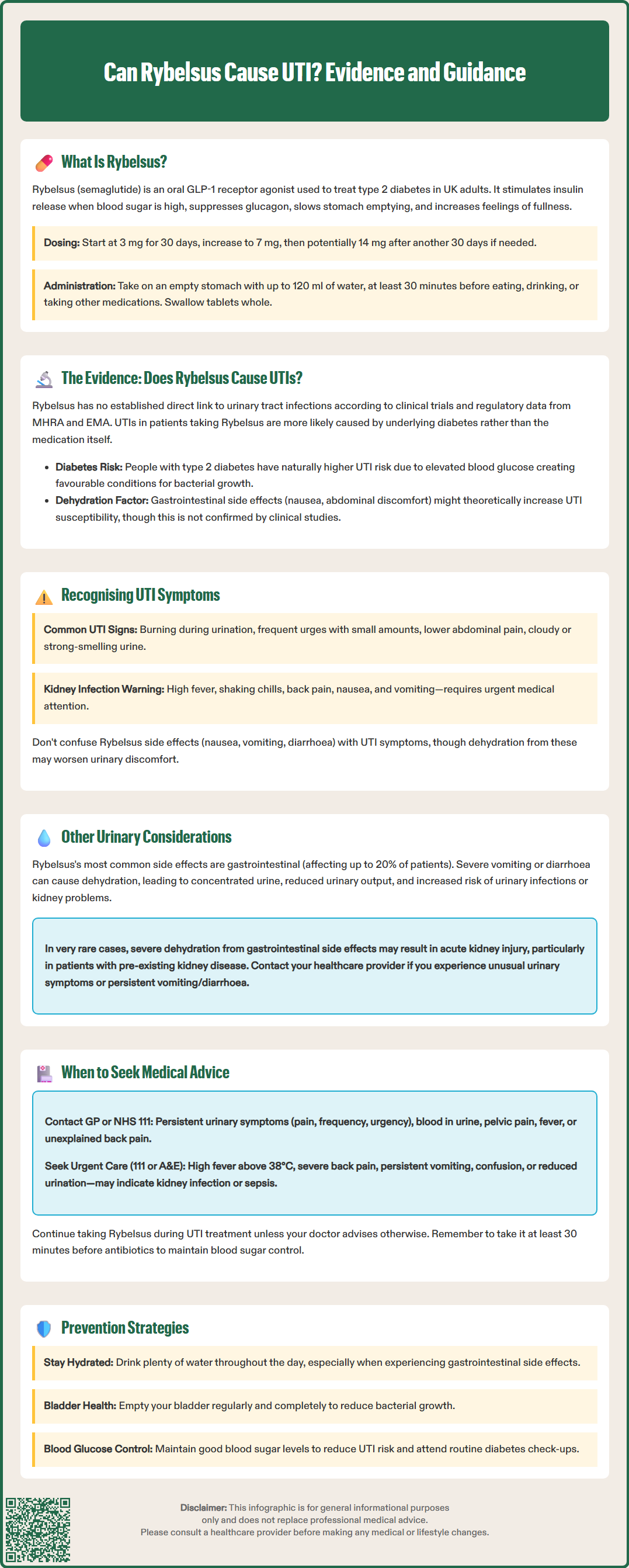
There is no established direct causal link between Rybelsus (semaglutide) and urinary tract infections (UTIs) based on current clinical evidence and regulatory data. The Summary of Product Characteristics (SmPC) approved by the MHRA and EMA does not list UTIs as a recognised adverse effect of semaglutide. In the pivotal clinical trials that led to Rybelsus's approval—including the PIONEER programme—UTIs were not reported at a significantly higher rate in patients taking semaglutide compared with those on placebo or comparator treatments, according to the European Public Assessment Report (EPAR).
However, it is important to recognise that people with type 2 diabetes are inherently at increased risk of developing UTIs, regardless of the medications they take. Elevated blood glucose levels can create a favourable environment for bacterial growth in the urinary tract, and diabetes-related complications such as incomplete bladder emptying (diabetic cystopathy) or reduced immune function can further elevate this risk. Therefore, if a patient taking Rybelsus develops a UTI, it is more likely attributable to their underlying diabetes rather than the medication itself.
Some patients may confuse gastrointestinal side effects—such as nausea, abdominal discomfort, or changes in bowel habit—with urinary symptoms, particularly if they are unfamiliar with the typical presentation of a UTI. Additionally, dehydration secondary to gastrointestinal upset (a common side effect of GLP-1 agonists) might hypothetically increase susceptibility to UTIs, though this remains speculative and not formally documented in clinical studies.
In summary, whilst Rybelsus does not directly cause UTIs, patients with diabetes should remain vigilant for urinary symptoms and maintain good glycaemic control, adequate hydration, and personal hygiene to minimise infection risk. If you suspect you are experiencing any adverse effects from Rybelsus, you can report these through the MHRA Yellow Card scheme.
A urinary tract infection (UTI) occurs when bacteria—most commonly Escherichia coli—invade the urinary system, which includes the bladder (cystitis), urethra (urethritis), or kidneys (pyelonephritis). Recognising the symptoms promptly is essential, as untreated UTIs can lead to more serious complications, particularly in individuals with diabetes.
Common symptoms of a lower UTI (cystitis) include:
Dysuria: a burning or stinging sensation when passing urine
Urinary frequency: needing to urinate more often than usual, often with only small amounts of urine passed
Urinary urgency: a sudden, compelling need to urinate
Suprapubic pain or discomfort: tenderness or pressure in the lower abdomen
Cloudy, dark, or strong-smelling urine: sometimes with visible blood (haematuria)
If the infection ascends to the kidneys (pyelonephritis), more severe symptoms may develop, including high fever, rigors (shaking chills), loin or back pain, nausea, and vomiting. This constitutes a medical emergency requiring urgent assessment.
For patients taking Rybelsus, it is important not to attribute urinary symptoms automatically to the medication. Gastrointestinal side effects—such as nausea, vomiting, or diarrhoea—are well-recognised with GLP-1 receptor agonists and typically occur early in treatment or after dose escalation. These should not be confused with UTI symptoms, though dehydration from gastrointestinal upset may exacerbate urinary discomfort.
If you experience any combination of the symptoms listed above, particularly if accompanied by fever or systemic unwellness, contact your GP or NHS 111 for assessment. Diagnosis is usually based on clinical symptoms, and a midstream urine sample may be sent for culture in certain situations (men, pregnant women, recurrent or atypical symptoms, treatment failure, or suspected upper UTI). It's important to note that visible haematuria that persists or recurs after treatment, or visible haematuria without UTI symptoms, warrants urgent referral to exclude urological cancer.
Whilst Rybelsus is not associated with UTIs, it is worth noting that urinary side effects are not prominently featured in the adverse event profile of semaglutide. The most commonly reported side effects of Rybelsus are gastrointestinal in nature, including nausea (occurring in up to 20% of patients), vomiting, diarrhoea, abdominal pain, constipation, and dyspepsia. These effects are usually mild to moderate, transient, and tend to diminish over time as the body adjusts to the medication.
That said, some patients may experience indirect urinary effects related to the drug's mechanism or secondary consequences of treatment:
Dehydration: Gastrointestinal side effects, particularly vomiting and diarrhoea, can lead to fluid loss. As noted in the SmPC, severe gastrointestinal adverse effects may lead to dehydration, which can result in concentrated urine, reduced urinary output, and potentially increased susceptibility to urinary infections or kidney strain. Maintaining adequate hydration is therefore essential.
Acute kidney injury (rare): In very rare cases, severe dehydration secondary to gastrointestinal side effects has been associated with acute kidney injury in patients taking GLP-1 receptor agonists. The SmPC recommends monitoring renal function in patients with pre-existing kidney disease or those at higher risk of dehydration.
If you notice any unusual urinary symptoms—such as significant changes in urine colour, volume, or frequency—whilst taking Rybelsus, discuss these with your healthcare provider. If you experience persistent vomiting or diarrhoea that impairs your ability to maintain hydration, contact a healthcare professional promptly, as temporary treatment interruption may be advised.
Remember to take Rybelsus at least 30 minutes before any other oral medicines, food or drink (other than water), and maintain adequate hydration throughout the day, especially if you experience gastrointestinal side effects.
Prompt recognition and treatment of a UTI is important for all patients, but particularly for those with diabetes, who are at higher risk of complications. You should contact your GP or NHS 111 if you experience:
Persistent or worsening dysuria, frequency, or urgency
Visible blood in the urine (haematuria)
Lower abdominal or pelvic pain
Fever, chills, or feeling generally unwell
New or unexplained back or loin pain
Seek urgent medical attention (via 111 or A&E) if you develop signs of an upper UTI or systemic infection, such as high fever (>38°C), severe back or flank pain, persistent vomiting, confusion, or reduced urine output. These may indicate pyelonephritis or sepsis, both of which require immediate assessment and intravenous antibiotics.
It's important to note that visible haematuria that persists or recurs after treatment for a UTI, or visible haematuria without UTI symptoms, warrants urgent referral to exclude urological cancer, in line with NICE guidance (NG12).
If you are taking Rybelsus and develop a UTI, do not stop your medication without consulting your healthcare team. Rybelsus can be continued during antibiotic treatment for a UTI, and maintaining glycaemic control is important for recovery. Remember to take Rybelsus at least 30 minutes before any other oral medicines, including antibiotics. If you are experiencing significant gastrointestinal side effects that are impairing your ability to eat, drink, or take medications, inform your doctor, as temporary dose adjustment or additional supportive measures may be needed.
Antibiotic choice and duration should follow NICE and local antimicrobial guidance. For uncomplicated lower UTIs, nitrofurantoin is often first-line if renal function permits (generally avoided if eGFR <45 mL/min), while trimethoprim is typically only used where there is low resistance risk or confirmed susceptibility. Men, pregnant women, and those with suspected pyelonephritis require urine culture and tailored management, often with longer antibiotic courses.
Finally, preventive measures are key: maintain good hydration, practice regular and complete bladder emptying, optimise blood glucose control, and attend routine diabetes reviews to monitor for complications.
No, there is no established direct causal link between Rybelsus (semaglutide) and urinary tract infections based on current clinical evidence and regulatory data. UTIs are not listed as a recognised adverse effect in the MHRA-approved Summary of Product Characteristics.
People with type 2 diabetes are inherently at increased risk of UTIs due to elevated blood glucose levels creating a favourable environment for bacterial growth, and diabetes-related complications such as incomplete bladder emptying or reduced immune function.
No, do not stop Rybelsus without consulting your healthcare team. Rybelsus can be continued during antibiotic treatment for a UTI, and maintaining glycaemic control is important for recovery.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.