
Can Wegovy cause heart palpitations? Whilst heart palpitations are not listed as a common side effect of Wegovy (semaglutide 2.4 mg) in clinical trials or the Summary of Product Characteristics, some patients report experiencing them during treatment. Wegovy is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. Understanding the relationship between Wegovy and cardiovascular symptoms, including palpitations, is essential for safe use. This article examines the evidence, explores potential mechanisms, and provides guidance on when to seek medical advice and how to manage symptoms whilst taking this medication.
Quick Answer: Wegovy is not officially linked to heart palpitations in clinical trials, though some patients may experience them due to rapid weight loss, dehydration, electrolyte imbalances, or the medication's effect on heart rate.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. Administered as a once-weekly subcutaneous injection, Wegovy works by mimicking the natural hormone GLP-1, which regulates appetite and food intake through actions on the brain's satiety centres.
The cardiovascular profile of semaglutide has been extensively studied, particularly through the SUSTAIN and SELECT trials. These landmark studies demonstrated that GLP-1 receptor agonists can reduce major adverse cardiovascular events (MACE) in people with established cardiovascular disease or multiple risk factors. The SELECT trial specifically showed that semaglutide 2.4 mg reduced the risk of cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke by 20% compared to placebo in people with pre-existing cardiovascular disease and overweight or obesity.
Despite these cardiovascular benefits, patients may experience various side effects during treatment. The most common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation, which typically diminish over time. Understanding the full spectrum of potential effects, including those affecting heart rhythm, is essential for both patients and healthcare professionals to ensure safe and effective use of this medication.
The MHRA and EMA have approved Wegovy with comprehensive safety data, and ongoing pharmacovigilance continues to monitor its real-world safety profile across diverse patient populations in the UK and Europe. According to NICE Technology Appraisal (TA875), Wegovy is recommended for use within NHS weight management services for a maximum duration of 2 years. Wegovy is contraindicated in pregnancy, personal or family history of medullary thyroid carcinoma, and multiple endocrine neoplasia syndrome type 2.
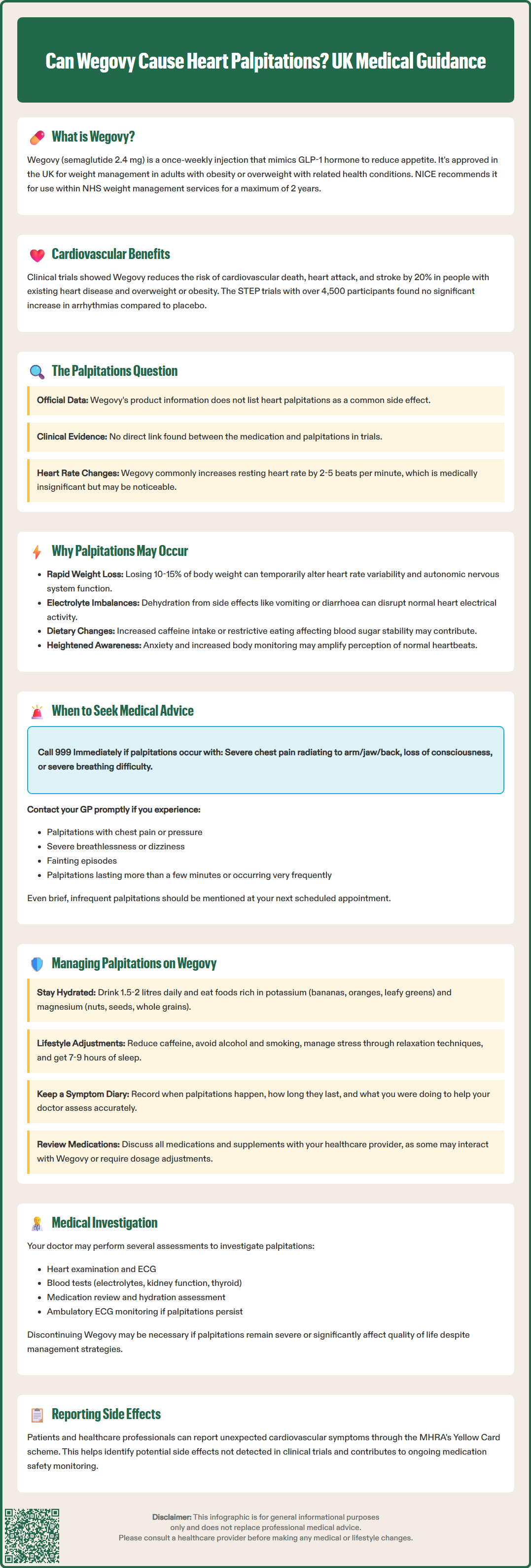
Heart palpitations—the sensation of a racing, pounding, fluttering, or irregular heartbeat—are not listed as a common side effect in Wegovy's Summary of Product Characteristics (SmPC) or patient information leaflet. However, there is no official direct link established between Wegovy and heart palpitations in the clinical trial data that supported its licensing.
In the pivotal STEP (Semaglutide Treatment Effect in People with obesity) clinical trials involving over 4,500 participants, palpitations were not reported as a frequent adverse event. The cardiovascular safety data from these trials showed that semaglutide was generally well-tolerated from a cardiac rhythm perspective, with no significant increase in arrhythmias compared to placebo.
The MHRA's Yellow Card scheme collects reports of suspected side effects, and both patients and healthcare professionals are encouraged to report any unexpected cardiovascular symptoms that may be associated with Wegovy treatment. This pharmacovigilance system helps identify potential safety signals that may not have been detected during clinical trials.
When palpitations occur in patients taking Wegovy, they may be multifactorial in origin rather than solely attributable to the medication itself. Factors such as rapid weight loss, changes in electrolyte balance, dehydration, dietary modifications, and pre-existing cardiac conditions may all contribute to the sensation of palpitations. Therefore, whilst palpitations can occur during Wegovy treatment, establishing causality requires careful clinical assessment and consideration of alternative explanations.
Several physiological mechanisms may explain why some patients experience palpitations whilst taking Wegovy, even though the medication itself does not directly cause arrhythmias. Understanding these mechanisms helps contextualise the symptom and guide appropriate management.
Rapid weight loss and metabolic changes represent a primary consideration. Wegovy typically induces substantial weight reduction—often 10-15% of body weight over several months. This rapid metabolic shift can affect cardiovascular physiology, including heart rate variability and autonomic nervous system function. As the body adapts to significant caloric restriction and weight loss, temporary alterations in cardiac rhythm perception may occur.
Dehydration and electrolyte imbalances commonly accompany GLP-1 receptor agonist therapy, particularly when gastrointestinal side effects such as vomiting or diarrhoea are present. Reduced fluid intake combined with increased fluid losses can lead to disturbances in sodium, potassium, and magnesium levels—all of which are crucial for normal cardiac electrical activity. Even mild electrolyte shifts can trigger palpitations in susceptible individuals.
Increased heart rate is a recognised pharmacological effect of GLP-1 receptor agonists. According to the Wegovy SmPC, increased heart rate is classified as a common side effect (affecting ≥1/100 to <1/10 patients). Clinical trials have documented modest increases in resting heart rate (typically 2-5 beats per minute) with semaglutide. Whilst this increase is generally clinically insignificant, some patients may become more aware of their heartbeat, particularly if they are monitoring their health closely during weight loss treatment.
Dietary changes and caffeine intake often accompany weight management programmes. Patients may inadvertently increase caffeine consumption or adopt restrictive eating patterns that affect blood glucose stability, both of which can contribute to palpitations. Additionally, anxiety and heightened body awareness during medical treatment may amplify the perception of normal cardiac activity, leading to increased reporting of palpitations that were previously unnoticed.
Whilst occasional palpitations are common and often benign, certain features warrant prompt medical evaluation. Patients should contact their GP or healthcare provider if palpitations are accompanied by:
Chest pain or pressure – this may indicate myocardial ischaemia or other serious cardiac conditions
Severe breathlessness – particularly if it occurs at rest or with minimal exertion
Dizziness, light-headedness, or syncope (fainting) – suggesting haemodynamic compromise
Palpitations lasting more than a few minutes or occurring very frequently throughout the day
Associated symptoms such as excessive sweating, nausea, or a sense of impending doom
Immediate medical attention (999 or A&E) is required if:
Palpitations are accompanied by severe chest pain, particularly if radiating to the arm, jaw, or back
There is sudden collapse or loss of consciousness
Severe difficulty breathing develops alongside palpitations
The patient has a known history of serious heart conditions
For urgent but non-emergency situations, patients should contact NHS 111 for advice.
For non-urgent palpitations that are brief, infrequent, and not associated with concerning symptoms, patients should still discuss them with their prescribing clinician at the next scheduled review. The healthcare provider may wish to:
Perform a cardiovascular examination and check vital signs, including heart rate and blood pressure
Arrange an electrocardiogram (ECG) to assess cardiac rhythm and exclude arrhythmias
Check electrolyte levels, renal function, and thyroid function through blood tests
Review medication history and assess for potential drug interactions
Evaluate hydration status and provide guidance on fluid intake
The NICE Clinical Knowledge Summary on palpitations recommends a thorough history, including the frequency, duration, and triggers of symptoms, alongside appropriate investigations to exclude significant cardiac pathology. Patients should maintain a symptom diary noting when palpitations occur, their duration, and any associated activities or symptoms, as this information aids clinical assessment.
If palpitations occur during Wegovy treatment and serious cardiac pathology has been excluded, several practical strategies can help manage symptoms whilst continuing weight loss therapy.
Optimising hydration and electrolyte balance is fundamental. Patients should aim for adequate fluid intake (typically 1.5-2 litres daily, unless otherwise advised for those with heart or renal conditions) and ensure a balanced diet rich in potassium (found in bananas, oranges, and leafy greens) and magnesium (present in nuts, seeds, and whole grains). If gastrointestinal side effects are prominent, oral rehydration solutions may be beneficial. Regular monitoring of electrolytes through blood tests may be appropriate for patients experiencing persistent symptoms, particularly those with chronic kidney disease who may need individualised dietary advice.
Lifestyle modifications can significantly reduce palpitation frequency:
Limit caffeine intake – reduce or eliminate coffee, tea, energy drinks, and chocolate, particularly in the afternoon and evening
Avoid alcohol and smoking – both can trigger palpitations and interact with cardiovascular function
Manage stress – incorporate relaxation techniques such as deep breathing exercises, mindfulness, or yoga
Ensure adequate sleep – aim for 7-9 hours nightly, as sleep deprivation can exacerbate palpitations
Gradual physical activity – avoid sudden intense exercise; build activity levels progressively
Medication review is essential. Healthcare providers should assess all concurrent medications, including over-the-counter preparations and supplements, as some may interact with Wegovy or independently cause palpitations. Dose adjustment of other medications, particularly those affecting heart rate or blood pressure, may be necessary as weight loss progresses.
Monitoring and follow-up should be individualised. Patients experiencing palpitations may benefit from more frequent clinical reviews during the initial months of treatment. Some may require ambulatory ECG monitoring (such as a 24-hour Holter monitor) to characterise the rhythm disturbance if symptoms persist.
If palpitations are severe, persistent, or significantly impact quality of life despite these measures, discontinuation of Wegovy may be considered in consultation with the prescribing clinician. However, this decision should be balanced against the cardiovascular benefits of sustained weight loss and the overall risk-benefit profile for the individual patient. Alternative weight management strategies, including other pharmacological options or referral to specialist weight management services, should be discussed if Wegovy is discontinued due to intolerable side effects.
Patients are encouraged to report any suspected side effects to the MHRA through the Yellow Card scheme (yellowcard.mhra.gov.uk).
No, heart palpitations are not listed as a common side effect in Wegovy's clinical trials or Summary of Product Characteristics. However, some patients may experience them due to factors such as rapid weight loss, dehydration, or electrolyte imbalances during treatment.
Seek immediate medical attention (999 or A&E) if palpitations occur with severe chest pain, collapse, or severe breathlessness. Contact your GP if palpitations are accompanied by chest discomfort, dizziness, syncope, or last more than a few minutes.
Ensure adequate hydration (1.5-2 litres daily), maintain balanced electrolyte intake, limit caffeine and alcohol, manage stress, and ensure adequate sleep. Your healthcare provider may arrange an ECG and blood tests to exclude serious causes and monitor electrolyte levels.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.