
Mounjaro (tirzepatide) is a dual GIP/GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus management. People living with multiple sclerosis (MS) may develop type 2 diabetes due to reduced mobility, corticosteroid use, or metabolic changes. When both conditions coexist, careful medication selection is essential to ensure diabetes treatments do not adversely interact with MS therapies or worsen neurological symptoms. Currently, no established link exists between Mounjaro and MS in terms of causing, improving, or exacerbating the condition. This article examines the evidence, safety considerations, and practical guidance for managing type 2 diabetes with Mounjaro in people with MS, aligned with UK clinical guidance.
Quick Answer: There is currently no established link between Mounjaro (tirzepatide) and multiple sclerosis, with no evidence suggesting the medication causes, worsens, or improves MS.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a relatively new medication licensed in the UK for the treatment of type 2 diabetes mellitus only. It is not indicated for type 1 diabetes or diabetic ketoacidosis. Administered as a once-weekly subcutaneous injection, it belongs to a novel class of medicines known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists. By activating both GIP and GLP-1 receptors, tirzepatide enhances insulin secretion when blood glucose levels are elevated, suppresses glucagon release, slows gastric emptying, and reduces appetite. These combined mechanisms help improve glycaemic control and often result in significant weight loss.
Multiple sclerosis (MS) is a chronic autoimmune neurological condition affecting the central nervous system. In MS, the immune system mistakenly attacks the protective myelin sheath surrounding nerve fibres, leading to inflammation, demyelination, and progressive neurological impairment. Symptoms vary widely and may include fatigue, mobility difficulties, visual disturbances, cognitive changes, and sensory problems. MS predominantly affects young to middle-aged adults and requires long-term management with disease-modifying therapies (DMTs), symptomatic treatments, and multidisciplinary support, as outlined in NICE guideline NG220.
People living with MS may develop other health conditions, including type 2 diabetes. Factors such as reduced physical activity due to mobility limitations, certain MS medications (particularly corticosteroids used during relapses), and metabolic changes can increase diabetes risk. When both conditions coexist, careful consideration is needed when selecting diabetes treatments to ensure they do not adversely interact with MS therapies or exacerbate neurological symptoms. Understanding how medications like Mounjaro fit into this complex clinical picture is essential for safe and effective management.
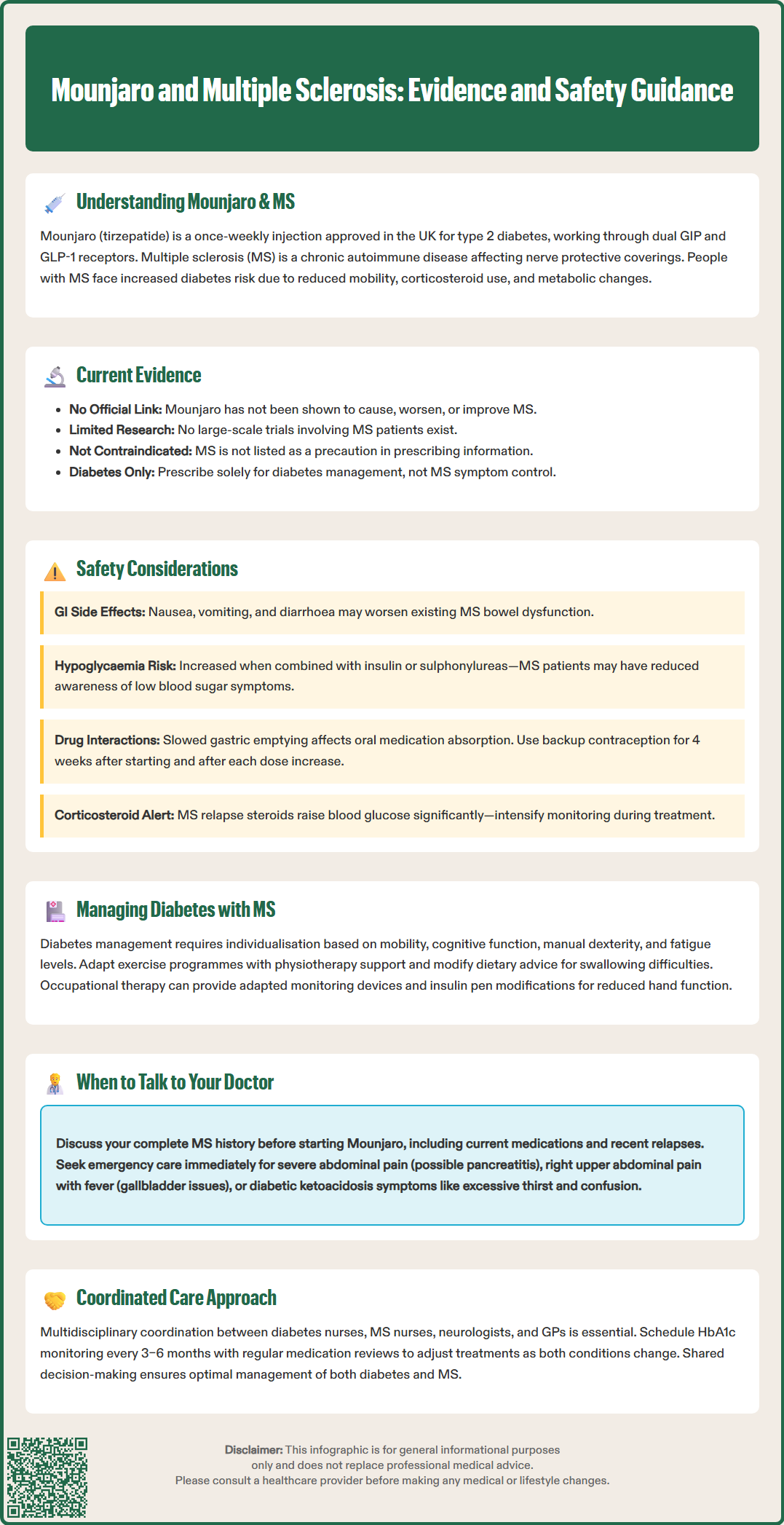
At present, there is no official link established between Mounjaro and multiple sclerosis in terms of the medication either causing, worsening, or improving MS. Tirzepatide has not been specifically studied in large-scale clinical trials involving people with MS, and the drug's prescribing information does not list MS as a contraindication or precaution. The pivotal trials that led to Mounjaro's approval (such as the SURPASS programme) primarily enrolled participants with type 2 diabetes but did not specifically focus on those with concurrent neurological conditions.
There is emerging interest in the potential neuroprotective effects of GLP-1 receptor agonists, a related class of medications. Some preclinical and early clinical research suggests that GLP-1 analogues may have anti-inflammatory and neuroprotective properties. However, these findings are predominantly from laboratory and animal studies, with limited human data. Tirzepatide's dual GIP/GLP-1 mechanism has not been extensively investigated in this context, and any potential benefits for MS remain entirely speculative and unproven.
Clinicians prescribing Mounjaro to patients with MS should rely on the established evidence base for type 2 diabetes management rather than expecting any direct impact on MS disease activity or progression. It is important to monitor patients closely for any unexpected neurological changes. While the UK SmPC does not contain MS-specific warnings, the absence of evidence is not evidence of absence, and clinical vigilance remains important. Healthcare professionals should report any suspected adverse reactions through the MHRA Yellow Card Scheme, contributing to ongoing pharmacovigilance and safety monitoring.
Patients with MS considering Mounjaro for diabetes management should be reassured that there is currently no evidence from clinical trials or regulatory assessments suggesting MS-specific harm, but equally, they should not expect the medication to influence their MS symptoms or disease course.
When prescribing Mounjaro to individuals with multiple sclerosis, several safety considerations warrant attention. Tirzepatide commonly causes gastrointestinal side effects, including nausea, vomiting, diarrhoea, and constipation, particularly during dose escalation. For people with MS who may already experience bowel dysfunction or neurogenic bladder issues, these adverse effects could compound existing symptoms and affect quality of life. Careful dose titration and symptomatic management strategies are essential. Caution is advised in patients with severe gastrointestinal disease, including gastroparesis.
The UK SmPC highlights several important safety warnings:
Pancreatitis: Patients should be educated about symptoms (severe abdominal pain, sometimes radiating to the back) and advised to stop tirzepatide immediately and seek urgent medical care if pancreatitis is suspected.
Gallbladder disease: Tirzepatide has been associated with an increased risk of cholelithiasis and cholecystitis. Patients should be alert to symptoms such as right upper quadrant pain, fever, or jaundice.
Acute kidney injury: Dehydration from severe gastrointestinal adverse effects may lead to acute kidney injury. Maintaining adequate hydration is important, particularly if experiencing persistent vomiting or diarrhoea.
Diabetic retinopathy: Rapid improvement in glycaemic control has been associated with temporary worsening of diabetic retinopathy. Patients with pre-existing retinopathy should be monitored closely, particularly if also using insulin.
Hypoglycaemia risk is generally low with Mounjaro when used alone, as its glucose-lowering effect is glucose-dependent. However, when combined with other diabetes medications such as sulphonylureas or insulin, the risk increases significantly. Dose reductions of these medications should be considered when initiating tirzepatide. People with MS may have altered awareness of hypoglycaemic symptoms due to autonomic dysfunction or sensory changes, making blood glucose monitoring particularly important.
Regarding drug interactions with MS disease-modifying therapies, there are no known direct pharmacokinetic or pharmacodynamic interactions between tirzepatide and commonly used DMTs such as interferons, glatiramer acetate, natalizumab, fingolimod, or ocrelizumab. However, because tirzepatide slows gastric emptying, it affects the absorption of oral medications. A clinically significant interaction exists with oral contraceptives; additional contraceptive methods are recommended for 4 weeks after initiation and for 4 weeks after each dose increase. Patients taking oral DMTs should be monitored for efficacy.
Corticosteroids, frequently used to treat MS relapses, can significantly elevate blood glucose levels and may necessitate temporary adjustments to diabetes therapy. Patients and healthcare teams should be prepared to intensify glucose monitoring during steroid courses.
Tirzepatide is contraindicated in pregnancy and breastfeeding. Women of childbearing potential should use effective contraception during treatment and stop tirzepatide at least 1 month before a planned pregnancy due to its extended half-life.
Managing type 2 diabetes in individuals with multiple sclerosis requires a holistic, patient-centred approach that addresses the unique challenges posed by both conditions. According to NICE guidelines (NG28), diabetes management should be individualised based on patient characteristics, comorbidities, and treatment tolerances. For people with MS, considerations include mobility limitations, cognitive function, manual dexterity for self-monitoring and injections, and the impact of fatigue on self-management behaviours.
Lifestyle modifications remain foundational but may require adaptation. Physical activity recommendations should account for MS-related disability, with physiotherapy input to develop safe, achievable exercise programmes. Dietary advice must consider swallowing difficulties (dysphagia) or gastrointestinal symptoms that some people with MS experience. Occupational therapy can assist with practical aspects of diabetes self-care, such as blood glucose monitoring devices or insulin pen adaptations for those with reduced hand function.
When selecting pharmacological treatments, NICE guidance recommends considering cardiovascular and renal risk profiles. SGLT2 inhibitors are preferred for those with heart failure or chronic kidney disease, while GLP-1 receptor agonists (including tirzepatide) may be considered for those with established cardiovascular disease. Medications that support weight management may be particularly beneficial, as obesity can worsen both diabetes control and MS-related mobility challenges. Tirzepatide may be considered where clinically appropriate and in line with NICE guidance. However, injectable therapies require adequate training and support, especially for patients with visual impairment, tremor, or cognitive difficulties that might affect technique.
Multidisciplinary coordination is essential. Diabetes specialist nurses, MS nurses, neurologists, and GPs should communicate regularly to ensure treatment plans are coherent and mutually reinforcing. Regular HbA1c monitoring (typically every 3–6 months) helps assess glycaemic control, whilst annual diabetes complications screening (retinopathy, nephropathy, foot checks) remains important. For patients with existing retinopathy, gradual rather than rapid improvement in HbA1c is advisable to reduce the risk of temporary worsening. People with MS may require more frequent reviews to address the dynamic nature of both conditions and optimise overall health outcomes and quality of life.
If you have multiple sclerosis and type 2 diabetes, or are considering Mounjaro as a treatment option, open communication with your healthcare team is vital. Before starting tirzepatide, discuss your complete medical history, including your MS diagnosis, current disease-modifying therapies, recent relapse history, and any MS-related symptoms that might affect diabetes management, such as fatigue, mobility issues, or cognitive changes.
Key questions to raise with your GP or diabetes specialist include:
Is Mounjaro suitable given my MS medications and overall health status?
How will we monitor for side effects, particularly gastrointestinal symptoms that might overlap with MS-related bowel dysfunction?
What are the signs of hypoglycaemia I should watch for, and how might MS affect my ability to recognise them?
Will Mounjaro interact with medications I take during MS relapses, such as corticosteroids?
What support is available to help me manage injections if I have difficulties with hand function or vision?
If I'm taking oral contraceptives, what additional contraceptive measures do I need?
What should I do if I'm planning pregnancy or breastfeeding?
How will we adjust my insulin or sulphonylurea doses to reduce hypoglycaemia risk?
When to seek urgent medical advice:
Stop taking tirzepatide and seek immediate medical attention if you experience symptoms of pancreatitis (severe abdominal pain, sometimes radiating to the back, with or without vomiting)
Contact your healthcare provider promptly if you develop gallbladder symptoms (pain in the right upper abdomen, fever, yellowing of skin/eyes)
Seek urgent care for unexplained neurological symptoms, severe or persistent gastrointestinal side effects, or signs of hypoglycaemia (confusion, sweating, tremor)
Get immediate help for symptoms of diabetic ketoacidosis (excessive thirst, frequent urination, abdominal pain, deep rapid breathing, drowsiness or confusion)
Contact your MS team if you experience a suspected MS relapse
Regular medication reviews ensure your treatment plan remains appropriate as both conditions evolve. Your healthcare team can adjust therapies, provide additional support services, and coordinate care between specialties. Remember, managing multiple long-term conditions requires partnership between you and your healthcare professionals, with shared decision-making at the heart of effective, personalised care.
There is currently no evidence from clinical trials or regulatory assessments suggesting that Mounjaro worsens MS symptoms or disease activity. However, gastrointestinal side effects may compound existing MS-related bowel dysfunction, requiring careful monitoring.
No known direct pharmacokinetic or pharmacodynamic interactions exist between tirzepatide and commonly used MS disease-modifying therapies such as interferons, glatiramer acetate, natalizumab, fingolimod, or ocrelizumab.
Yes, inform your healthcare team about your MS diagnosis, current disease-modifying therapies, and any MS-related symptoms that might affect diabetes management, such as mobility issues, cognitive changes, or bowel dysfunction, to ensure safe and coordinated care.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.