Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly prescribed for weight management in the UK. Whilst these medications offer significant benefits for weight reduction, they can cause gastrointestinal side effects, with constipation being one of the most commonly reported. Understanding why constipation occurs, how to manage it effectively, and when to seek medical advice is essential for patients considering or currently using these treatments. This article explores the mechanisms behind constipation with weight loss injections and provides practical guidance aligned with UK clinical practice.
Quick Answer: Weight loss injections can cause constipation by slowing gastrointestinal motility and reducing food intake, affecting approximately 15-24% of patients using GLP-1 receptor agonists.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections prescribed in the UK typically belong to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists. These include semaglutide (marketed as Wegovy for weight management) and liraglutide (Saxenda). Ozempic (semaglutide) is licensed only for type 2 diabetes treatment, not for weight loss. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved these medications for specific indications, and NICE provides guidance on their use within the NHS.
These medications work by mimicking a naturally occurring hormone called GLP-1, which is released by the intestines after eating. When administered as an injection—usually once weekly for semaglutide or once daily for liraglutide—they bind to GLP-1 receptors throughout the body, particularly in the pancreas, brain, and gastrointestinal tract. This binding triggers several physiological responses that contribute to weight loss.
The primary mechanisms include:
Appetite suppression: GLP-1 receptor agonists act on areas of the brain that regulate hunger and satiety, reducing appetite and food cravings
Delayed gastric emptying: These medications slow the rate at which food leaves the stomach, promoting feelings of fullness for longer periods
Enhanced insulin secretion: In response to food intake, they stimulate glucose-dependent insulin release from the pancreas, which helps regulate blood glucose levels
Reduced glucagon secretion: They suppress glucagon (a hormone that raises blood sugar) in a glucose-dependent manner, further improving glycaemic control
The slowing of gastric emptying and effects on gut motility are central to both the therapeutic benefits and the gastrointestinal side effects commonly experienced with these medications. Understanding these mechanisms helps explain why constipation is a recognised adverse effect of GLP-1 receptor agonists.
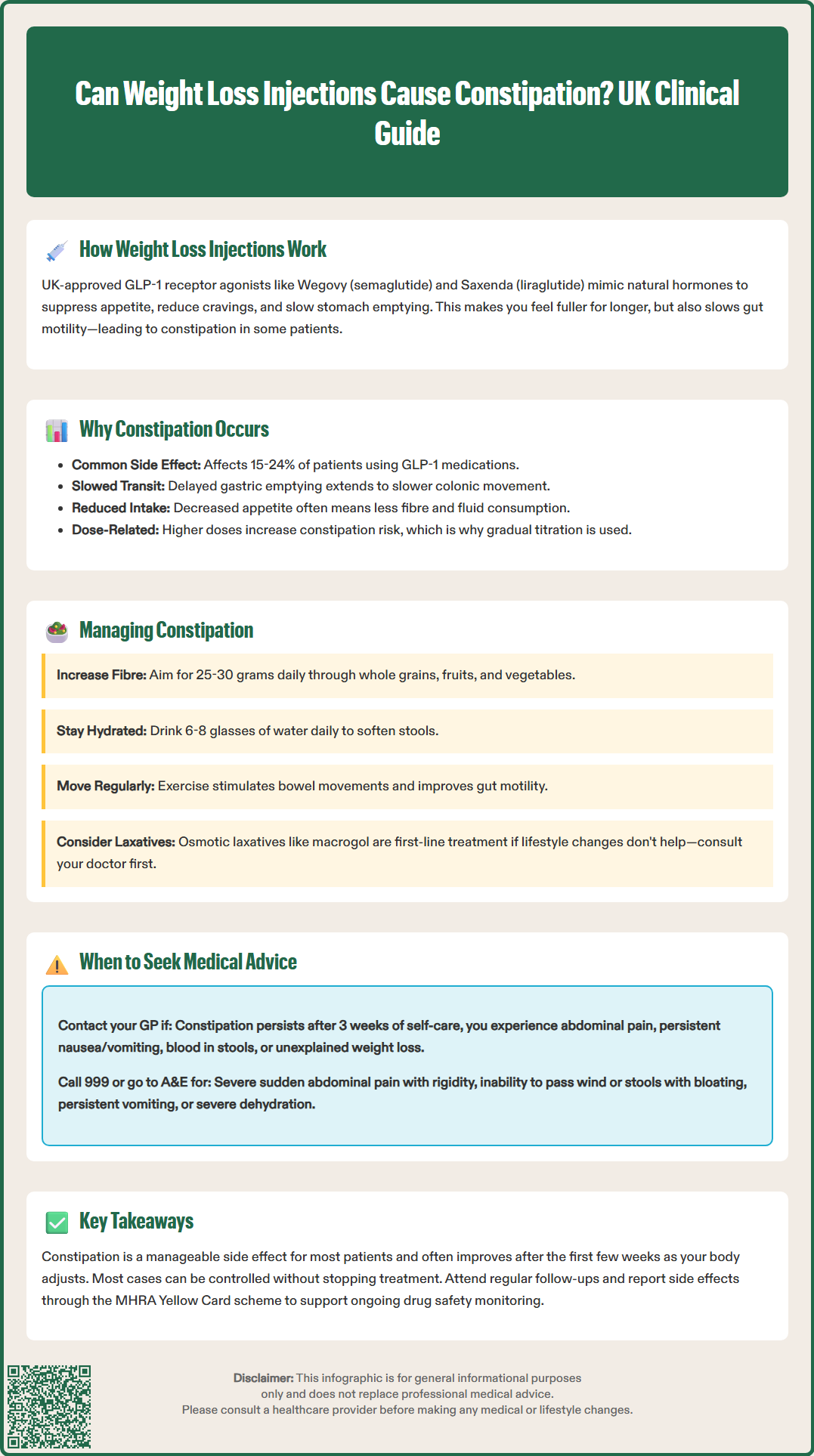
Constipation is one of the most frequently reported gastrointestinal side effects of weight loss injections, affecting a significant proportion of patients using GLP-1 receptor agonists. Clinical trials have documented constipation rates of approximately 24% with semaglutide 2.4mg (Wegovy) in the STEP trials and 15-20% with liraglutide 3.0mg (Saxenda), though individual experiences vary considerably.
The primary reason constipation develops relates to the medication's effect on gastrointestinal motility. GLP-1 receptors are present throughout the digestive tract, and when activated by these medications, they slow the movement of food and waste through the intestines. Whilst delayed gastric emptying contributes to satiety and weight loss, this same mechanism can lead to slower colonic transit times, resulting in harder, less frequent stools.
Several contributing factors compound this effect:
Reduced food and fluid intake: As appetite decreases, patients often consume less food and may inadvertently reduce their fluid intake, both of which can contribute to constipation
Dietary changes: Many patients alter their eating patterns significantly when starting weight loss treatment, sometimes reducing fibre intake or changing meal timing
Decreased physical bulk: Lower food volume means less material moving through the digestive system, which can slow transit further
The severity of constipation typically correlates with the dose of medication. When treatment is initiated, healthcare providers usually start with a lower dose and gradually increase it over several weeks, as specified in the product SmPCs. This titration approach helps minimise gastrointestinal side effects, including constipation. However, some patients may experience persistent bowel changes even at maintenance doses.
It is important to note that whilst constipation is common, serious gastrointestinal complications are rare. The SmPCs for these medications do include post-marketing reports of cases such as intestinal obstruction, though causality has not been definitively established.
Effective management of constipation whilst using weight loss injections involves a combination of lifestyle modifications and, when necessary, appropriate use of laxatives. Most cases can be successfully managed without discontinuing treatment, allowing patients to continue benefiting from the weight loss effects.
Dietary and lifestyle interventions should be the first-line approach:
Increase fibre intake: Aim for 25–30 grams of fibre daily through wholegrains, fruits, vegetables, pulses, and seeds. Introduce fibre gradually to avoid bloating
Maintain adequate hydration: Drink 6-8 glasses of fluid daily (around 1.5-2 litres), adjusting for individual factors including any heart or kidney conditions
Regular physical activity: Exercise stimulates intestinal motility and can help maintain regular bowel movements
Establish a routine: Try to use the toilet at the same time each day, particularly after meals when the gastrocolic reflex is strongest
Respond to urges promptly: Don't delay when you feel the need to open your bowels
When lifestyle measures prove insufficient, pharmacological options may be appropriate:
Osmotic laxatives (such as macrogol) are often considered first-line for hard stools and work by drawing water into the bowel
Bulk-forming laxatives (such as ispaghula husk) may be helpful for some patients but should be taken with plenty of fluid
Stimulant laxatives (such as senna or bisacodyl) may be used short-term for more persistent constipation, but should not be relied upon long-term
Patients should consult their GP or prescribing clinician before starting any laxative regimen, particularly if taking other medications. Importantly, do not use laxatives if you have severe abdominal pain, vomiting, or suspected bowel obstruction—seek medical advice instead. If constipation persists despite treatment, your prescriber may consider slowing the dose titration, temporarily pausing, or reducing your medication dose.
It's worth noting that some patients find their bowel habits normalise after the first few weeks of treatment as their body adjusts to the medication. Keeping a symptom diary can help identify patterns and triggers, which can be valuable information when discussing management strategies with healthcare professionals.
Whilst mild to moderate constipation is a recognised and manageable side effect of weight loss injections, certain symptoms warrant prompt medical attention. Patients should be aware of warning signs that may indicate more serious complications requiring clinical assessment.
Contact your GP or prescribing clinician if:
Your constipation has not improved after trying self-care measures and over-the-counter laxatives for around 3 weeks
You have abdominal pain: Particularly if it's persistent, worsening, or accompanied by distension
You experience nausea and vomiting: Especially if persistent or preventing adequate fluid intake
You notice blood in stools: Either bright red blood or black, tarry stools
You have unexplained weight loss: Beyond what is expected from the treatment programme
You develop a fever: Which may indicate infection or inflammation
Contact NHS 111 or seek urgent medical attention if:
Your symptoms are severe or getting worse rapidly
You're unable to keep fluids down
You have signs of dehydration (dizziness, reduced urination, confusion)
Seek emergency medical attention (A&E or call 999) if you develop:
Severe, sudden abdominal pain with rigidity
Inability to pass wind or stools with progressive abdominal distension
Persistent vomiting preventing fluid intake
Severe dehydration or confusion
Patients and healthcare professionals can report suspected side effects of medications through the MHRA Yellow Card scheme. This helps authorities monitor the safety of medicines and identify any new risks.
Patients should maintain regular follow-up appointments with their prescribing clinician, typically scheduled every few months during weight loss treatment. These consultations provide opportunities to discuss any bowel changes, adjust management strategies, or consider dose modifications if side effects become problematic. In some cases, if constipation proves severe and unmanageable despite appropriate interventions, switching to an alternative weight management approach may be necessary. Open communication with healthcare providers ensures that treatment remains both effective and tolerable, maximising the benefits whilst minimising adverse effects.
Constipation affects approximately 15-24% of patients using GLP-1 receptor agonists for weight loss, with rates varying between different medications and doses. Clinical trials show semaglutide 2.4mg (Wegovy) causes constipation in around 24% of patients, whilst liraglutide 3.0mg (Saxenda) affects 15-20%.
Many patients find their bowel habits normalise after the first few weeks as their body adjusts to the medication. If constipation persists, lifestyle modifications and appropriate laxatives can usually manage symptoms effectively without needing to stop treatment.
Osmotic laxatives such as macrogol are often considered first-line treatment for constipation related to GLP-1 medications, as they work by drawing water into the bowel. Patients should consult their GP or prescribing clinician before starting any laxative regimen to ensure appropriate selection and dosing.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.