
Do weight loss injections cause cancer? This question has emerged as GLP-1 receptor agonists like semaglutide (Wegovy, Ozempic) and liraglutide (Saxenda) have become increasingly prescribed for obesity and type 2 diabetes management in the UK. Concerns stem primarily from animal studies showing thyroid tumours in rodents, leading to regulatory warnings. However, large-scale human clinical trials and real-world evidence have not demonstrated a causal link between these medications and cancer. Understanding the distinction between preclinical findings and human data is essential for patients and clinicians making informed treatment decisions. This article examines current evidence, regulatory guidance, and safety considerations surrounding GLP-1 agonists and cancer risk.
Quick Answer: Current evidence does not establish that weight loss injections cause cancer in humans, despite precautionary warnings based on animal studies showing thyroid tumours in rodents.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections, particularly glucagon-like peptide-1 (GLP-1) receptor agonists, have become increasingly popular for managing obesity and type 2 diabetes. In the UK, semaglutide 2.4mg (Wegovy) and liraglutide 3mg (Saxenda) are licensed for weight management, while semaglutide at lower doses (Ozempic) is licensed only for type 2 diabetes treatment. As their use has expanded, questions have emerged regarding potential cancer risks, particularly following pre-clinical studies and post-marketing surveillance reports.
These medications work by mimicking the natural hormone GLP-1, which regulates appetite and blood glucose levels. By activating GLP-1 receptors in the brain, pancreas, and gastrointestinal tract, they reduce hunger, slow gastric emptying, and improve insulin secretion. Whilst these mechanisms are well-established for weight management, concerns about cancer risk stem primarily from animal studies showing thyroid C-cell tumours in rodents exposed to high doses of GLP-1 agonists.
It is crucial to understand that there is no definitive evidence establishing a direct causal link between GLP-1 medications and cancer in humans. However, regulatory bodies including the Medicines and Healthcare products Regulatory Agency (MHRA) and the European Medicines Agency (EMA) have included precautionary warnings in product information based on preclinical findings, leading to contraindications in patients with certain risk factors.
Patients considering or currently using weight loss injections should be aware of these concerns whilst recognising that ongoing pharmacovigilance continues to monitor safety. Understanding the distinction between animal study findings and human clinical evidence is essential for informed decision-making regarding these treatments.
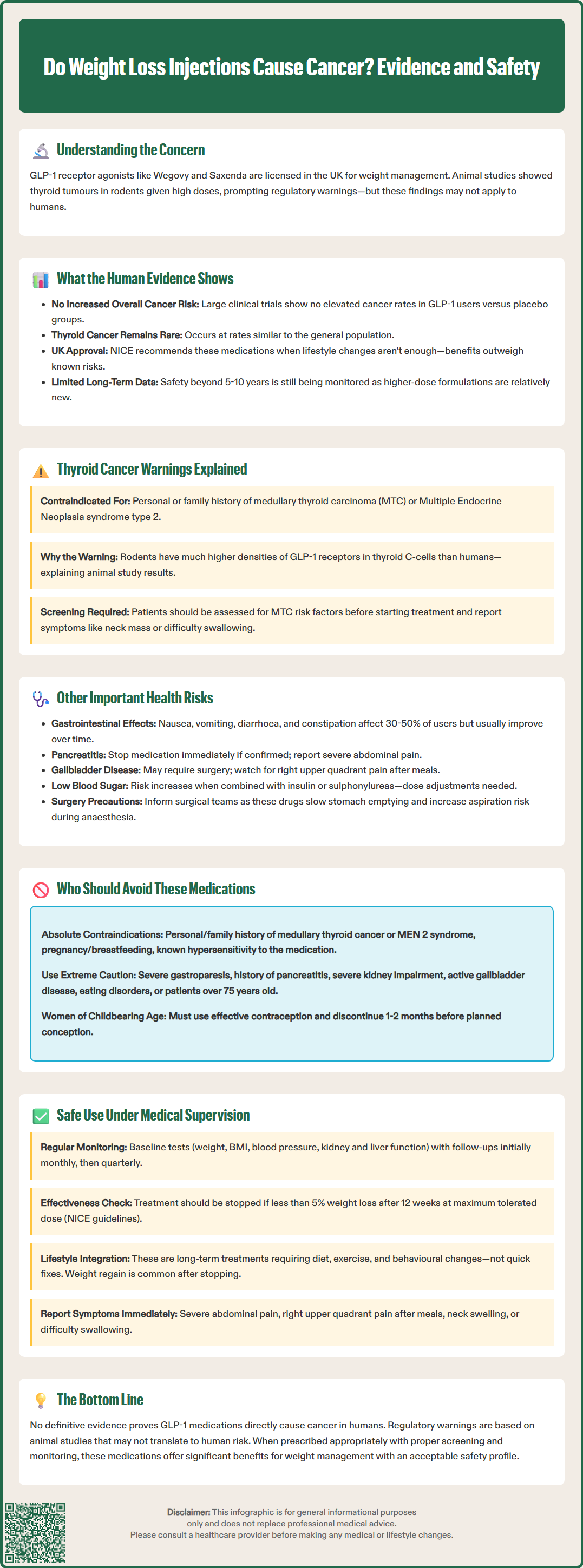
Large-scale clinical trials and real-world studies have not demonstrated an increased overall cancer risk in humans taking GLP-1 receptor agonists. The STEP trials for semaglutide and the SCALE trials for liraglutide, involving thousands of participants over extended periods, showed no significant elevation in cancer incidence compared to placebo groups. Meta-analyses examining cardiovascular outcomes trials have similarly found no concerning cancer signals across diverse patient populations.
Key findings from human studies include:
No statistically significant increase in overall cancer rates among GLP-1 users
Thyroid cancer cases remain extremely rare, with incidence rates comparable to background population rates
Some observational studies suggest potential associations with reduced risk of certain obesity-related cancers, though these findings are hypothesis-generating and require further investigation
Long-term safety data continue to accumulate through post-marketing surveillance
The National Institute for Health and Care Excellence (NICE) acknowledges these findings in its technology appraisals for weight management medications. NICE TA875 (semaglutide 2.4mg) and TA664 (liraglutide 3mg) recommend these GLP-1 agonists as appropriate treatment options when lifestyle interventions prove insufficient, balancing potential benefits against known risks.
However, the relatively recent introduction of higher-dose formulations for weight management means that very long-term data (beyond 5–10 years) remain limited. Ongoing registry studies and pharmacovigilance programmes, including the EMA's Pharmacovigilance Risk Assessment Committee (PRAC) and the MHRA's Yellow Card scheme, continue monitoring for rare adverse events, including malignancies. Healthcare professionals should counsel patients that whilst current evidence is reassuring, continued surveillance remains important as clinical experience with these medications expands across broader populations and longer treatment durations.
The most prominent cancer-related warning for GLP-1 receptor agonists concerns medullary thyroid carcinoma (MTC), a rare form of thyroid cancer. This warning stems from rodent studies where semaglutide and liraglutide caused dose-dependent thyroid C-cell tumours, including carcinomas. Rodents have substantially higher densities of GLP-1 receptors in thyroid C-cells compared to humans, which may explain this species-specific finding.
Regulatory contraindications include:
Personal history of medullary thyroid carcinoma
Family history of MTC
Multiple endocrine neoplasia syndrome type 2 (MEN 2)
Known hypersensitivity to the medication or its components
The MHRA and EMA require prominent warnings in product information (SmPCs), and prescribers must screen patients for these risk factors before initiating treatment. Patients should be counselled about symptoms of thyroid tumours, including a neck mass, dysphagia (difficulty swallowing), dyspnoea (shortness of breath), or persistent hoarseness.
Despite these precautionary measures, there is no established causal relationship between GLP-1 agonists and MTC in humans. Post-marketing surveillance has identified isolated cases, but these occur at rates consistent with background population incidence. The European Medicines Agency's Pharmacovigilance Risk Assessment Committee has reviewed available data and concluded that current evidence does not support a definitive link.
Patients with thyroid nodules or elevated calcitonin levels detected during routine screening should undergo appropriate endocrinological evaluation before considering GLP-1 therapy. However, routine calcitonin screening or thyroid ultrasound is not recommended for all patients, as stated in the product SmPCs, as its predictive value in asymptomatic individuals remains uncertain and may lead to unnecessary investigations.
Beyond cancer concerns, GLP-1 receptor agonists carry several established adverse effects that require clinical consideration. The most common side effects are gastrointestinal, affecting approximately 30-50% of users (varying by product and dose according to SmPCs), including nausea, vomiting, diarrhoea, constipation, and abdominal pain. These typically diminish over time as tolerance develops, though some patients discontinue treatment due to persistent symptoms.
Significant clinical risks include:
Pancreatitis: Acute inflammation of the pancreas has been reported, though causality remains debated. Patients should seek immediate medical attention for severe, persistent abdominal pain radiating to the back. Treatment should be discontinued if pancreatitis is suspected or confirmed, and not restarted if pancreatitis is confirmed.
Gallbladder disease: Rapid weight loss increases cholelithiasis (gallstone) risk. Cholecystitis and cholelithiasis occur more frequently in GLP-1 users, potentially requiring surgical intervention.
Hypoglycaemia: When combined with insulin or sulphonylureas, blood glucose may drop dangerously low. Dose adjustments of concomitant medications are often necessary.
Diabetic retinopathy complications: Rapid glycaemic improvement may temporarily worsen retinopathy in patients with pre-existing disease.
Renal impairment: Dehydration from gastrointestinal side effects can precipitate acute kidney injury, particularly in vulnerable patients. GLP-1 agonists should be used with caution in severe renal impairment with careful monitoring.
Recent pharmacovigilance reports have also highlighted concerns about gastroparesis (delayed gastric emptying) and potential aspiration risks during anaesthesia. The Royal College of Anaesthetists and Association of Anaesthetists have issued guidance recommending patients inform surgical teams about GLP-1 use, as prolonged gastric retention may necessitate modified fasting protocols.
Patients should maintain adequate hydration, report persistent symptoms promptly, and attend regular monitoring appointments. Suspected adverse reactions should be reported through the MHRA Yellow Card scheme. Healthcare professionals should conduct baseline assessments including renal function and liver enzymes, with additional tests such as lipase or thyroid function where clinically indicated, with ongoing surveillance tailored to individual risk profiles.
Certain patient groups should not use GLP-1 receptor agonists due to established contraindications or insufficient safety data. Prescribers must conduct thorough medical histories and risk assessments before initiating treatment, adhering to MHRA-approved product characteristics and NICE guidance.
Absolute contraindications include:
Personal or family history of medullary thyroid carcinoma
Multiple endocrine neoplasia syndrome type 2 (MEN 2)
Pregnancy and breastfeeding (limited human data; potential fetal risks)
Known hypersensitivity to semaglutide, liraglutide, or excipients
Relative contraindications and cautions:
Severe gastroparesis
History of pancreatitis (use with extreme caution; some clinicians consider this a contraindication)
Severe renal impairment (use with caution; monitor for dehydration and acute kidney injury; limited data in end-stage renal disease)
Active gallbladder disease
Proliferative diabetic retinopathy or maculopathy requiring acute treatment
Type 1 diabetes or diabetic ketoacidosis (GLP-1 agonists are not indicated for these conditions)
Age under 18 years (product-specific; check current SmPC as some formulations have specific adolescent indications)
Patients with eating disorders, body dysmorphia, or unrealistic weight loss expectations may not be appropriate candidates. Psychological assessment should form part of comprehensive obesity management, as recommended in NICE guidance CG189.
Elderly patients (over 75 years) require careful consideration due to limited clinical trial data, increased frailty, and polypharmacy concerns. Dose titration should be particularly cautious, with close monitoring for adverse effects including dehydration and malnutrition.
Women of childbearing potential should use effective contraception during treatment. For semaglutide, the SmPC advises discontinuation at least two months before planned conception; for liraglutide, at least one month before. Any patient experiencing concerning symptoms should contact their GP or prescribing clinician promptly rather than abruptly stopping medication without medical guidance.
Weight loss injections should only be prescribed and monitored by appropriately qualified healthcare professionals within structured weight management programmes. NICE recommends GLP-1 agonists as part of comprehensive obesity management, incorporating dietary modification, increased physical activity, and behavioural interventions alongside pharmacotherapy.
Essential monitoring components include:
Baseline assessment: Weight, BMI, waist circumference, blood pressure, HbA1c (if diabetic), renal function, liver function, and other tests where clinically indicated
Regular follow-up: Initially monthly, then quarterly once stable, assessing weight loss progress, tolerability, and adherence
Treatment response evaluation: Product-specific stopping rules apply. NICE TA875 recommends discontinuing semaglutide 2.4mg if <5% weight loss after 12 weeks at maximum tolerated dose; NICE TA664 recommends discontinuing liraglutide 3mg if <5% weight loss after 12 weeks at full dose
Adverse event surveillance: Systematic enquiry about gastrointestinal symptoms, abdominal pain, visual changes, and other concerning features
Medication review: Adjustment of concomitant diabetes medications to prevent hypoglycaemia
Patient safety advice:
Patients should be counselled to report immediately any symptoms suggesting pancreatitis (severe abdominal pain), gallbladder disease (right upper quadrant pain, particularly after meals), or thyroid masses (neck swelling, difficulty swallowing). They should maintain adequate hydration, particularly during initial titration when nausea is most prominent.
Prescribers should provide clear written information about injection technique, storage requirements (refrigeration before first use; product-specific in-use storage conditions), and disposal of sharps. Patients must understand that these medications represent long-term treatment rather than short-term solutions, with weight regain common after discontinuation.
The NHS typically provides GLP-1 agonists through specialist weight management services (Tier 3/4) or diabetes clinics, following NICE TA875 and TA664 criteria, ensuring appropriate patient selection and monitoring. Private prescribing has expanded significantly, raising concerns about inadequate screening and follow-up. Patients obtaining these medications through private or online services should ensure their provider conducts thorough medical assessments and offers ongoing clinical supervision.
Patients should be advised to report suspected adverse reactions via the MHRA Yellow Card scheme. Ultimately, whilst current evidence does not support cancer causation in humans, responsible prescribing requires individualised risk-benefit assessment, informed consent, and vigilant post-marketing surveillance to detect rare adverse events as clinical experience continues to evolve.
Large-scale clinical trials and real-world studies have not demonstrated an increased overall cancer risk in humans taking GLP-1 receptor agonists. Whilst animal studies showed thyroid tumours in rodents, post-marketing surveillance in humans has not confirmed a causal link, though ongoing monitoring continues.
Patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2) should not use these medications. These contraindications are based on precautionary principles from animal studies, and prescribers must screen for these risk factors before initiating treatment.
Report immediately any neck mass, difficulty swallowing, persistent hoarseness, severe abdominal pain, or right upper quadrant pain. Whilst these symptoms are rare, prompt medical evaluation ensures appropriate investigation and management of potential complications.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.