
GLP-1 receptor agonists, including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda), are increasingly prescribed for type 2 diabetes and weight management. As their use expands, questions have emerged about whether GLP-1 medications cause vision problems. Clinical evidence suggests that whilst these medicines do not directly damage the eyes, they may be associated with worsening diabetic retinopathy in certain patients, particularly those with pre-existing eye disease who experience rapid improvements in blood glucose control. Understanding this relationship, recognising warning signs, and maintaining appropriate eye surveillance are essential for anyone taking these treatments.
Quick Answer: GLP-1 receptor agonists do not directly cause vision problems, but may worsen diabetic retinopathy in patients with pre-existing eye disease who experience rapid blood glucose improvements.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily prescribed for type 2 diabetes mellitus and, in specific formulations, for weight management. These medicines include semaglutide (Ozempic for diabetes; Wegovy for weight management), dulaglutide (Trulicity for diabetes), liraglutide (Victoza for diabetes; Saxenda for weight management), and exenatide (Byetta, Bydureon for diabetes). They work by mimicking the action of a naturally occurring hormone called GLP-1, which is released from the intestine after eating.
The mechanism of action involves several complementary pathways. GLP-1 receptor agonists stimulate insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning they only promote insulin release when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared to some other diabetes medications. Simultaneously, these drugs suppress glucagon secretion, a hormone that raises blood glucose, thereby preventing excessive glucose production by the liver.
Additionally, GLP-1 medications slow gastric emptying, which helps moderate the post-meal rise in blood glucose and promotes satiety. They also act on appetite centres in the brain, reducing hunger and food intake, which explains their effectiveness in weight management. The combined effect is improved glycaemic control, often accompanied by significant weight loss. Some GLP-1 receptor agonists have also demonstrated cardiovascular benefits in clinical trials, though this varies between agents.
In the UK, NICE recommends GLP-1 receptor agonists as second- or third-line treatment options for type 2 diabetes when metformin and other oral agents have not achieved adequate control (NICE NG28). They may be considered earlier in people with a BMI ≥35 kg/m² (adjusted for ethnicity) or for whom weight loss would benefit other obesity-related comorbidities. Their use has expanded considerably, and with increased prescribing comes greater awareness of potential adverse effects, including questions about their impact on vision.
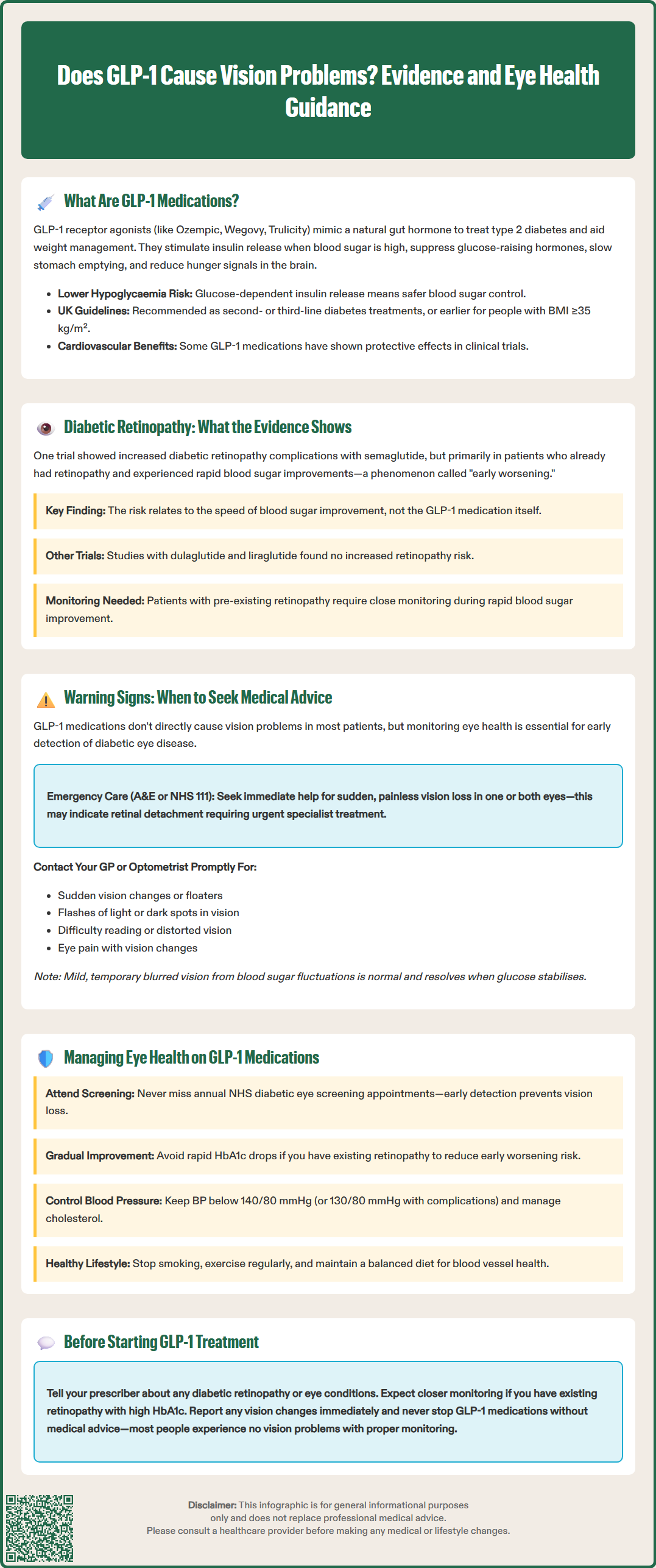
The relationship between GLP-1 receptor agonists and vision problems centres primarily on diabetic retinopathy, a complication of diabetes affecting the blood vessels in the retina. Clinical trial data have produced mixed findings that require careful interpretation.
The SUSTAIN-6 trial, which evaluated semaglutide in patients with type 2 diabetes at high cardiovascular risk, identified a statistically significant increase in diabetic retinopathy complications in the semaglutide group compared to placebo. However, subsequent analysis revealed important context: the increased risk was predominantly observed in patients with pre-existing diabetic retinopathy and those who experienced rapid improvements in glycaemic control. The magnitude of HbA1c reduction, rather than the medication itself, appeared to be the critical factor.
This phenomenon is well-recognised in diabetes management. Rapid lowering of blood glucose after prolonged periods of poor control can temporarily worsen diabetic retinopathy—a condition sometimes called "early worsening". This effect was previously documented in the DCCT and UKPDS trials and occurs regardless of the treatment method used (insulin, oral agents, or GLP-1 medications), reflecting changes in retinal blood flow and vascular permeability during metabolic adjustment.
Subsequent trials, including REWIND (dulaglutide) and LEADER (liraglutide), did not demonstrate increased retinopathy risk. Current evidence suggests that the risk of vision problems with GLP-1 medications appears primarily related to rapid glycaemic improvement in patients with pre-existing retinopathy rather than a direct medication effect across all patients.
The MHRA and EMA have reviewed this evidence, and the Summary of Product Characteristics (SmPC) for semaglutide (Ozempic, Wegovy) specifically advises that patients with diabetic retinopathy should be closely monitored during treatment, particularly during periods of rapid glycaemic improvement. This monitoring is especially important for patients using insulin concurrently. The SmPCs for other GLP-1 receptor agonists contain similar precautionary advice.
Whilst GLP-1 medications do not directly cause vision problems in most patients, anyone taking these treatments should remain vigilant about eye health, particularly if they have diabetes. Early detection of diabetic eye disease is crucial for preventing permanent vision loss.
Contact your GP or optometrist promptly if you experience:
Sudden vision changes, including blurred vision, floaters (dark spots or strings), or flashes of light
Progressive difficulty reading or recognising faces
Dark or empty areas in your visual field
Distorted vision, where straight lines appear wavy
Eye pain or redness accompanied by vision changes
Difficulty with night vision or colour perception
If you experience sudden, painless vision loss in one or both eyes, this constitutes an ophthalmological emergency. You should attend your local eye casualty department or A&E immediately, or call NHS 111 for urgent advice. These symptoms may indicate retinal detachment, vitreous haemorrhage, or vascular occlusion—all of which require urgent specialist assessment.
It is important to note that mild, temporary blurred vision can occur when blood glucose levels fluctuate, even in the absence of retinopathy. This happens because glucose changes affect the lens of the eye, altering its refractive properties. Such symptoms typically resolve once glucose levels stabilise and do not indicate permanent damage.
Before starting GLP-1 treatment, inform your prescriber if you have any history of diabetic retinopathy or other eye conditions. If you have known diabetic retinopathy, your healthcare team may recommend an eye examination and closer monitoring during the initial months of treatment, particularly if your HbA1c is significantly elevated. The NHS Diabetic Eye Screening Programme offers regular retinal photography to all people with diabetes aged 12 and over—ensure you attend these appointments regularly.
Protecting your vision whilst taking GLP-1 receptor agonists involves a comprehensive approach to diabetes management and regular eye surveillance. The following strategies can help minimise any potential risks.
Attend regular diabetic eye screening appointments. The NHS Diabetic Eye Screening Programme provides annual digital retinal photography, which can detect early changes before symptoms develop. If retinopathy is identified, you may be referred to hospital eye services for closer monitoring or treatment. Do not miss these appointments—early intervention with laser therapy or intravitreal injections can prevent vision loss.
Optimise your overall diabetes control gradually. Whilst improved glycaemic control is the goal, avoiding large and rapid HbA1c reductions may reduce the risk of early worsening in patients with existing retinopathy. Your diabetes team will balance the benefits of glucose lowering against this consideration, potentially adjusting medication doses more conservatively if you have advanced eye disease.
Maintain good blood pressure and cholesterol control. Hypertension and dyslipidaemia independently contribute to diabetic retinopathy progression. NICE guidelines (NG28) recommend blood pressure targets below 140/80 mmHg (or 130/80 mmHg if kidney, eye, or cerebrovascular damage is present) and lipid management according to cardiovascular risk.
Adopt a healthy lifestyle. Smoking significantly increases retinopathy risk and should be avoided. Regular physical activity and a balanced diet support both glycaemic control and vascular health. The weight loss often achieved with GLP-1 medications provides additional metabolic benefits.
Communicate with your healthcare team. Report any vision changes promptly and ensure your GP, diabetes specialist, and optometrist are aware of all your medications. If you develop new or worsening retinopathy, your diabetes team may adjust your treatment plan. Do not stop taking GLP-1 medications without consulting your healthcare provider, as the overall benefits for diabetes control, weight management, and cardiovascular protection typically outweigh the manageable risk of retinopathy progression in susceptible individuals.
If you suspect any adverse effects from your medication, including vision changes, you can report these through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Remember that most people taking GLP-1 medications experience no vision problems, particularly when appropriate monitoring and gradual glycaemic improvement are implemented.
GLP-1 medications do not directly damage the eyes, but may worsen pre-existing diabetic retinopathy in patients who experience rapid blood glucose improvements. Most people taking these treatments experience no vision problems, particularly with appropriate monitoring.
Contact your GP or optometrist promptly if you experience sudden vision changes, blurred vision, floaters, flashes of light, dark areas in your visual field, or distorted vision. Sudden painless vision loss requires immediate emergency assessment.
Yes, attending annual NHS Diabetic Eye Screening appointments is essential for all people with diabetes taking GLP-1 medications. Early detection through regular retinal photography can identify changes before symptoms develop and prevent vision loss.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.