
Glucagon-like peptide-1 (GLP-1) receptor agonists, such as semaglutide and liraglutide, are medications licensed in the UK for managing type 2 diabetes and obesity. Recent research has explored whether these drugs might influence addictive behaviours, as GLP-1 receptors are found in brain regions involved in reward processing. Whilst animal studies suggest potential effects on substance-seeking behaviour, clinical evidence in humans remains preliminary and inconsistent. Currently, GLP-1 receptor agonists are not approved or recommended by NICE for treating addiction. This article examines the emerging research, safety considerations, and what to discuss with your GP if you have questions about GLP-1 medications and substance use disorders.
Quick Answer: GLP-1 receptor agonists are not currently approved for addiction treatment in the UK, and whilst early research shows potential effects on reward pathways, clinical evidence remains insufficient to support their use for substance use disorders.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed to manage type 2 diabetes mellitus and, more recently, obesity. These drugs mimic the action of naturally occurring GLP-1, an incretin hormone produced in the intestine following food intake. GLP-1 plays a crucial role in glucose homeostasis by stimulating insulin secretion in a glucose-dependent manner, suppressing glucagon release, and slowing gastric emptying.
Commonly prescribed GLP-1 receptor agonists in the UK include semaglutide (Ozempic, Wegovy, and oral Rybelsus), liraglutide (Victoza, Saxenda), dulaglutide (Trulicity), and exenatide (Byetta, Bydureon). Most are administered via subcutaneous injection, with dosing frequencies ranging from daily to once weekly depending on the specific formulation, though oral semaglutide (Rybelsus) is taken daily by mouth. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved these agents primarily for glycaemic control in type 2 diabetes (not type 1 diabetes or diabetic ketoacidosis), with only semaglutide (Wegovy) and liraglutide (Saxenda) licensed for weight management in adults with obesity or overweight with weight-related comorbidities.
Beyond their metabolic effects, GLP-1 receptor agonists have demonstrated effects on appetite regulation and reward pathways in the brain. GLP-1 receptors are expressed not only in pancreatic tissue but also in various brain regions, including areas involved in reward processing, such as the nucleus accumbens and ventral tegmental area. This neurological distribution has prompted researchers to investigate whether these medications might influence addictive behaviours beyond their established indications. Whilst GLP-1 receptor agonists are not currently licensed for addiction treatment in the UK, emerging preclinical and clinical evidence has generated interest in their potential role in substance use disorders.
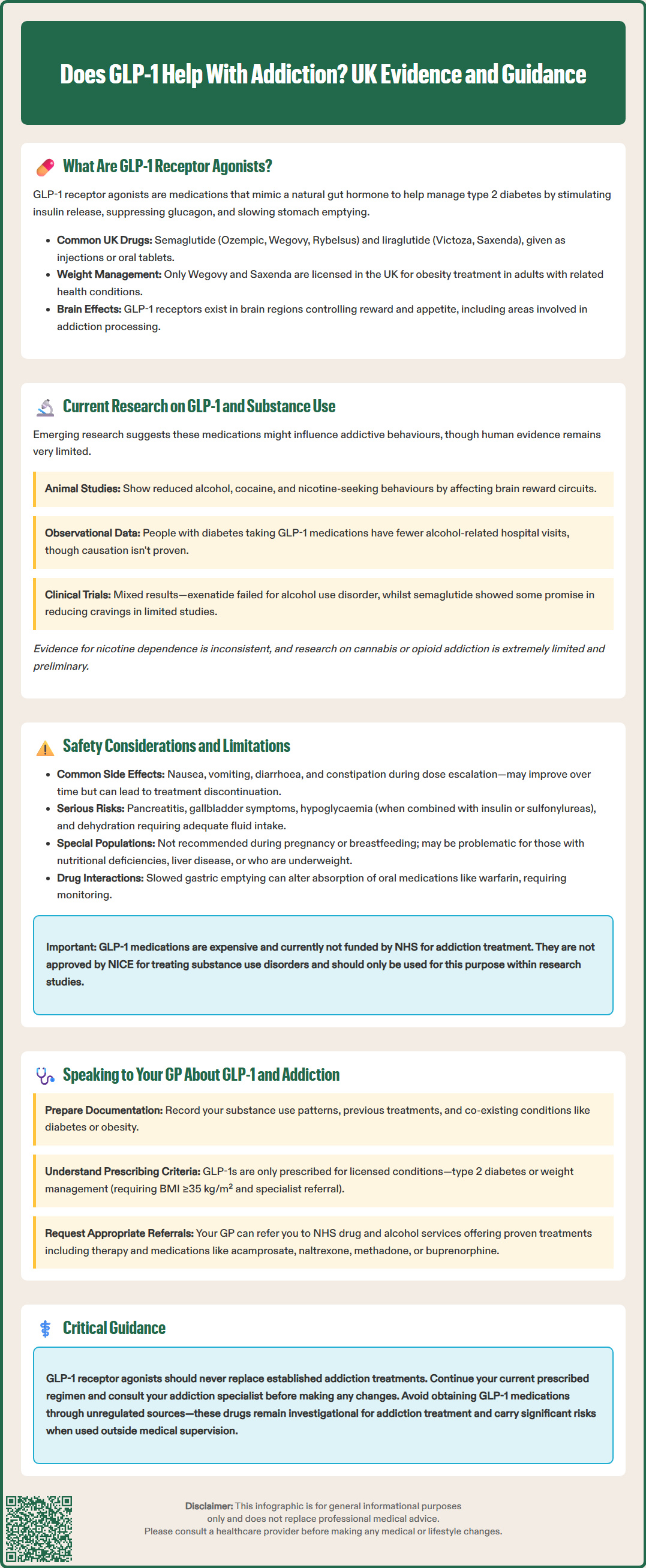
Preclinical studies in animal models have provided intriguing evidence that GLP-1 receptor agonists may reduce reward-seeking behaviours associated with various substances. Research in rodents has demonstrated that administration of GLP-1 analogues can decrease alcohol consumption, reduce cocaine self-administration, and diminish nicotine-seeking behaviour. These effects appear to be mediated through modulation of dopaminergic reward circuits, particularly in the mesolimbic pathway, which is central to addiction neurobiology.
Clinical evidence in humans remains preliminary and limited. Several observational studies have examined real-world data from patients prescribed GLP-1 receptor agonists for diabetes or obesity. A notable retrospective cohort study published in 2022 analysed electronic health records and found that individuals with type 2 diabetes and alcohol use disorder who were prescribed GLP-1 receptor agonists had lower rates of alcohol-related hospital encounters compared to those on other diabetes medications. However, such observational findings cannot establish causality and may be subject to confounding factors.
Small-scale clinical trials are now underway to prospectively evaluate GLP-1 receptor agonists for addiction treatment. Results have been mixed. For example, a randomised controlled trial of once-weekly exenatide for alcohol use disorder failed to meet its primary outcomes. Early-phase studies investigating semaglutide for alcohol use disorder have reported reductions in alcohol craving and consumption in some participants, but these trials typically involve small sample sizes and short follow-up periods. Research into nicotine dependence has shown inconsistent results, with some studies suggesting reduced cigarette consumption whilst others found no significant effect. Evidence for effects on cannabis or opioid use disorders is even more limited and preliminary.
It is important to emphasise that there is no official indication for GLP-1 receptor agonists in treating substance use disorders. NICE guidance does not currently recommend these medications for addiction management, and further robust, randomised controlled trials are needed to establish efficacy, optimal dosing, and long-term safety in this context. At present, use of GLP-1 receptor agonists for addiction should be limited to research settings.
Common adverse effects of GLP-1 receptor agonists include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation, which typically occur during dose escalation and may diminish over time. These side effects can be significant enough to cause treatment discontinuation in some patients. Other reported adverse reactions include injection site reactions, headache, fatigue, and dizziness. More serious but rare complications include pancreatitis, gallbladder disease, and potential thyroid C-cell tumours (observed in rodent studies, though human relevance remains uncertain).
Patients should be advised to seek immediate medical attention if they experience severe, persistent abdominal pain (which may indicate pancreatitis) or symptoms of gallbladder disease. When used with insulin or sulfonylureas, GLP-1 receptor agonists may increase the risk of hypoglycaemia, requiring dose adjustments of these medications. Rapid improvement in glycaemic control with semaglutide may worsen diabetic retinopathy in some patients with type 2 diabetes. Dehydration and acute kidney injury can occur, particularly with gastrointestinal side effects, so adequate fluid intake is important. These medications are not recommended during pregnancy or breastfeeding, and women of childbearing potential should use effective contraception.
When considering GLP-1 receptor agonists in the context of addiction, several important limitations must be acknowledged. Firstly, individuals with active substance use disorders may have complex medical and psychiatric comorbidities that could complicate treatment. The gastrointestinal side effects of GLP-1 analogues might be particularly problematic in patients with alcohol use disorder who may already experience nutritional deficiencies or liver disease. Additionally, the significant weight loss associated with these medications may not be appropriate for all individuals with addiction, particularly those who are already underweight.
Drug interactions warrant careful consideration. Whilst GLP-1 receptor agonists have relatively few direct pharmacokinetic interactions, their effect on gastric emptying can alter the absorption of some oral medications. This is most notable with immediate-release exenatide. Monitoring may be needed when initiating or adjusting doses of concurrent medications with a narrow therapeutic index, such as warfarin (with INR monitoring).
Cost and accessibility represent practical barriers. GLP-1 receptor agonists are expensive medications, and NHS prescribing is currently restricted to licensed indications (type 2 diabetes and, in limited circumstances, obesity management). Off-label use for addiction would not typically be funded, and private prescription costs may be prohibitive for many patients. Furthermore, the current evidence base is insufficient to support routine clinical use for substance use disorders outside of research settings.
If you experience any side effects while taking these medications, report them to your healthcare professional and consider reporting suspected adverse reactions via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
If you are interested in discussing GLP-1 receptor agonists in relation to addiction concerns, preparation for your GP appointment can facilitate a productive conversation. Consider documenting your substance use patterns, previous treatment attempts, and any co-existing medical conditions such as diabetes or obesity that might make you eligible for these medications under their licensed indications. Be honest and specific about your concerns, as this enables your GP to provide tailored advice and appropriate referrals.
Your GP will need to assess whether you meet criteria for a licensed GLP-1 receptor agonist prescription. For type 2 diabetes, NICE guidance (NG28) recommends considering these agents in specific circumstances, including when metformin is contraindicated or not tolerated, when additional glucose-lowering therapy is needed, or when a drug with proven cardiovascular benefit is appropriate. For weight management, eligibility is defined by NICE technology appraisals (TA875 for semaglutide/Wegovy and TA664 for liraglutide/Saxenda) and typically requires referral to specialist weight management services. Criteria generally include a BMI ≥35 kg/m² (or lower with adjustments for certain ethnic backgrounds and comorbidities) and previous unsuccessful weight management attempts. Treatment duration is limited under NHS criteria.
Referral to specialist services is essential for comprehensive addiction management. Your GP can refer you to local NHS drug and alcohol services, which offer evidence-based treatments including psychological interventions (such as cognitive behavioural therapy and motivational interviewing) and, where appropriate, pharmacological treatments with established efficacy. For alcohol dependence, these include acamprosate, naltrexone (used off-label in the UK), and in selected cases, disulfiram. For opioid dependence, methadone or buprenorphine maintenance therapy may be appropriate. NHS smoking cessation services can provide support and medications for tobacco dependence. You can find local addiction services through the NHS website.
It is crucial to understand that GLP-1 receptor agonists should not replace established addiction treatments. If you are currently receiving treatment for substance use disorder, continue with your prescribed regimen and discuss any changes with your addiction specialist. Self-medication or obtaining GLP-1 analogues through unregulated sources carries significant risks and is not advisable. Whilst research into GLP-1 receptor agonists for addiction is ongoing, these medications remain investigational for this purpose, and clinical decisions should be guided by current evidence-based guidelines and individual patient circumstances.
No, GLP-1 receptor agonists are not approved or recommended by NICE for treating substance use disorders. They are licensed only for type 2 diabetes and obesity management, and use for addiction should be limited to research settings.
Animal studies suggest GLP-1 receptor agonists may reduce substance-seeking behaviour, but human clinical trials have produced inconsistent results. Whilst some observational studies and small trials report reduced alcohol consumption or craving, robust evidence is lacking and further research is needed.
You can discuss GLP-1 receptor agonists with your GP if you meet criteria for their licensed indications (type 2 diabetes or obesity), but they should not replace established addiction treatments. Your GP can refer you to specialist NHS addiction services for evidence-based interventions.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.