Many patients prescribed Ozempic wonder whether this diabetes medication contains caffeine, particularly if they experience side effects such as nausea or changes in heart rate. The straightforward answer is no—Ozempic (semaglutide) does not contain caffeine or any caffeine-related compounds. This prescription medicine is a glucagon-like peptide-1 (GLP-1) receptor agonist used to improve blood sugar control in adults with type 2 diabetes mellitus. Its formulation includes semaglutide as the active ingredient, alongside inactive excipients that stabilise the medication. Understanding what Ozempic contains, how it works, and whether you can safely consume caffeine whilst taking it can help you manage your treatment confidently and address any concerns with your healthcare provider.
Quick Answer: Ozempic does not contain caffeine; it contains only semaglutide as the active ingredient, a GLP-1 receptor agonist for type 2 diabetes.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereNo, Ozempic does not contain caffeine. This is a common question among patients prescribed this medication, likely arising from concerns about potential interactions or side effects that might overlap with caffeine consumption.
Ozempic (semaglutide) is a prescription medicine used to improve blood sugar control in adults with type 2 diabetes mellitus. The formulation contains semaglutide as the active pharmaceutical ingredient, along with several inactive excipients that help stabilise and deliver the medication. None of these components include caffeine or any caffeine-related compounds, as confirmed by the official Summary of Product Characteristics (SmPC) available on the electronic Medicines Compendium (eMC).
The confusion may stem from certain side effects of Ozempic—such as nausea, a small mean increase in heart rate (a class effect of GLP-1 receptor agonists), or changes in energy levels—which can sometimes be mistakenly attributed to stimulant-like substances. However, these effects result from semaglutide's mechanism of action on glucose regulation and gastric emptying, not from any stimulant properties.
It is important to understand that Ozempic works through an entirely different pathway than caffeine. Whilst caffeine is a central nervous system stimulant that affects adenosine receptors, semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist that influences insulin secretion, glucagon suppression, and appetite regulation. If you have concerns about the ingredients in your medication or experience unexpected symptoms, consult your GP or pharmacist, who can provide detailed information about the formulation and address any specific worries you may have regarding your treatment.
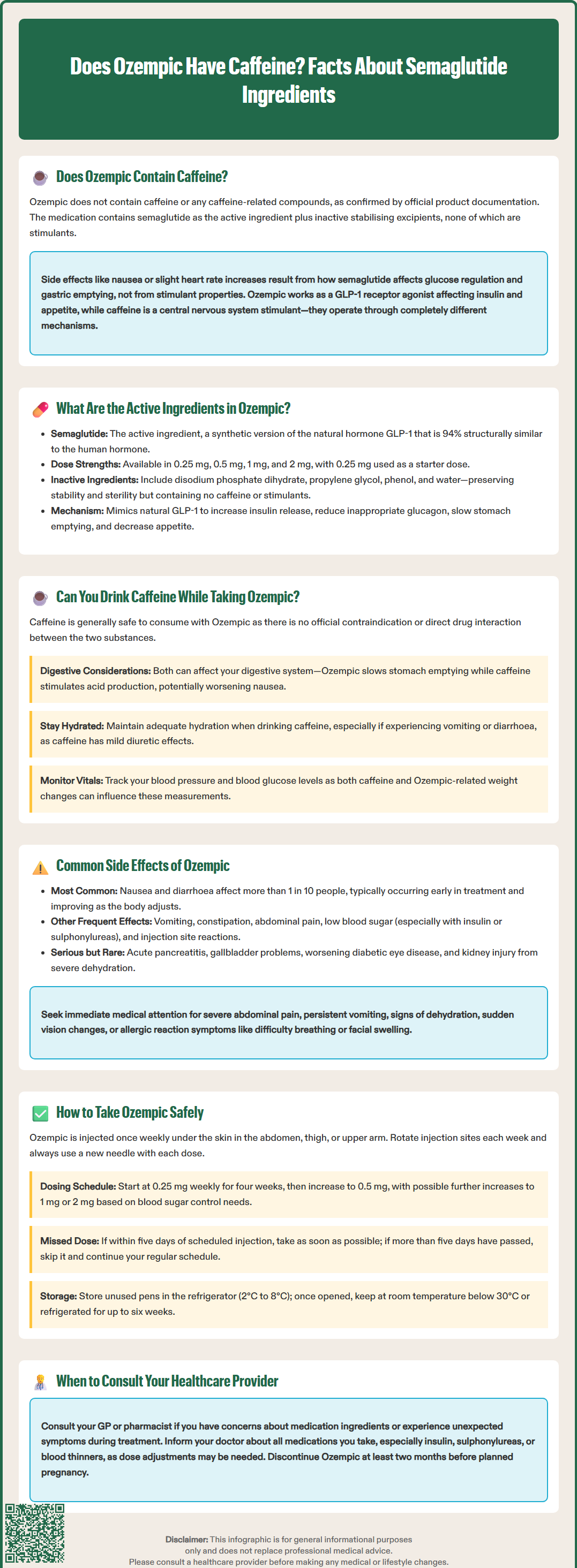
The sole active ingredient in Ozempic is semaglutide, a synthetic analogue of human glucagon-like peptide-1 (GLP-1). Semaglutide is manufactured through recombinant DNA technology and shares 94% structural similarity with native human GLP-1, with specific modifications that extend its duration of action.
Each Ozempic pre-filled pen contains semaglutide at varying concentrations depending on the prescribed dose. The medication is available in four strengths in the UK: 0.25 mg, 0.5 mg, 1 mg, and 2 mg per injection. The 0.25 mg dose is typically used as an initial dose to help the body adjust to the medication, whilst 0.5 mg, 1 mg, and 2 mg are maintenance doses used for ongoing blood glucose control.
Inactive ingredients (excipients) in Ozempic include:
Disodium phosphate dihydrate
Propylene glycol
Phenol
Water for injections
Hydrochloric acid and sodium hydroxide (for pH adjustment)
These excipients serve important pharmaceutical functions: they maintain the stability of semaglutide in solution, preserve the sterility of the injectable formulation, and ensure the medication remains effective throughout its shelf life. None of these components have stimulant properties or contain caffeine, as documented in the Ozempic SmPC.
Semaglutide's pharmacological action centres on mimicking the effects of natural GLP-1, a hormone released by the intestine in response to food intake. By activating GLP-1 receptors, semaglutide enhances insulin secretion when blood glucose levels are elevated, suppresses inappropriate glucagon release, slows gastric emptying, and reduces appetite. This multi-faceted mechanism makes it effective for glycaemic control in type 2 diabetes, and it has also been approved at higher doses (under the brand name Wegovy) for weight management in specific patient populations, accessed through specialist weight management services according to NICE technology appraisal guidance.
Yes, you can generally consume caffeine whilst taking Ozempic. There is no official contraindication or direct pharmacological interaction between semaglutide and caffeine. The Medicines and Healthcare products Regulatory Agency (MHRA) and the electronic Medicines Compendium (eMC) do not list caffeine as a substance that should be avoided during Ozempic treatment, as confirmed in the interactions section of the SmPC.
However, it is worth considering how caffeine consumption might indirectly affect your experience with Ozempic. Both substances can influence gastrointestinal function, though through different mechanisms. Ozempic slows gastric emptying as part of its therapeutic action, which can lead to feelings of fullness, nausea, or indigestion—particularly when treatment is first initiated or the dose is increased. Caffeine, especially in large quantities, can stimulate gastric acid secretion and may exacerbate gastrointestinal discomfort in some individuals.
Practical considerations for caffeine consumption whilst on Ozempic:
Monitor your tolerance: If you experience nausea or stomach upset with Ozempic, you may find that reducing caffeine intake or consuming it with food helps minimise discomfort.
Stay hydrated: If you experience vomiting or diarrhoea with Ozempic, you may be at risk of dehydration. Caffeine has mild diuretic effects (primarily at high doses or in non-habitual users), so ensure adequate water intake, particularly if you experience any gastrointestinal side effects.
Blood pressure awareness: Whilst there is no direct interaction, both caffeine and changes in body weight (which may occur with Ozempic) can influence blood pressure. If you have hypertension, discuss your caffeine consumption with your healthcare provider.
Blood glucose monitoring: Individual responses to caffeine vary, with some people experiencing temporary effects on blood glucose. Continue regular monitoring as advised by your diabetes care team.
If you notice any unusual symptoms after consuming caffeine whilst taking Ozempic, or if you have specific concerns about dietary interactions, consult your GP or diabetes specialist nurse for personalised advice.
Like all medicines, Ozempic can cause side effects, although not everyone experiences them. Understanding potential adverse effects helps patients recognise what is normal and when to seek medical advice.
Very common side effects (affecting more than 1 in 10 people):
Nausea: This is the most frequently reported side effect, particularly during the initial weeks of treatment or following dose increases. It typically improves over time as the body adjusts.
Diarrhoea: Gastrointestinal disturbances are common due to semaglutide's effect on gastric emptying and gut motility.
Common side effects (affecting up to 1 in 10 people):
Vomiting
Constipation
Abdominal pain or discomfort
Dyspepsia (indigestion)
Decreased appetite
Hypoglycaemia (low blood sugar), particularly when used in combination with insulin or sulphonylureas
Injection site reactions (redness, itching, or bruising)
Less common but important side effects:
Acute pancreatitis: Characterised by severe, persistent abdominal pain that may radiate to the back. This requires immediate medical attention.
Gallbladder problems: Including gallstones (cholelithiasis) and inflammation (cholecystitis), which may present as right upper abdominal pain, particularly after eating.
Diabetic retinopathy complications: Patients with pre-existing diabetic eye disease should have regular ophthalmology reviews, as rapid improvement in blood glucose control can temporarily worsen retinopathy.
Acute kidney injury: Usually in the context of severe dehydration from vomiting or diarrhoea.
When to seek immediate medical attention:
Contact your GP urgently or attend A&E if you experience severe abdominal pain, persistent vomiting preventing fluid intake, signs of dehydration, symptoms of pancreatitis, or sudden changes in vision. Call 999 or go to A&E immediately if you experience symptoms of a severe allergic reaction such as difficulty breathing, swelling of the face or throat, or severe skin rash. For concerns about hypoglycaemia management or adjusting concurrent diabetes medications, contact your diabetes care team promptly. Most side effects are manageable with supportive measures and often diminish with continued treatment.
If you experience any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed above. You can also report side effects directly via the Yellow Card Scheme at yellowcard.mhra.gov.uk to help provide more information on the safety of this medicine.
Ozempic is administered as a subcutaneous injection once weekly, on the same day each week, at any time of day, with or without meals. Proper administration technique and adherence to safety guidance are essential for optimal therapeutic outcomes and minimising adverse effects.
Administration technique:
Ozempic comes in a pre-filled, multi-dose pen designed for ease of use. Your healthcare provider or diabetes specialist nurse should demonstrate proper injection technique before you begin treatment.
Injection sites include the abdomen, thigh, or upper arm. Rotate injection sites each week to reduce the risk of local skin reactions and injection site nodules.
Always use a new needle for each injection and dispose of used needles in a sharps container.
Check the medication before injecting—it should be clear and colourless. Do not use if the solution appears cloudy, discoloured, or contains particles.
Dosing schedule:
Treatment typically begins with 0.25 mg once weekly for four weeks. This initial dose is not therapeutically effective for glycaemic control but allows your body to adjust to the medication, reducing the likelihood of gastrointestinal side effects. After four weeks, the dose is increased to 0.5 mg once weekly. If additional blood glucose control is needed after at least four weeks on 0.5 mg, your doctor may increase the dose to 1 mg once weekly. For patients requiring further glycaemic control, the dose may be increased to a maximum of 2 mg once weekly after at least four weeks on the 1 mg dose.
Important safety considerations:
Missed dose: If you miss a dose and it has been less than five days since the scheduled injection, administer it as soon as possible. If more than five days have passed, skip the missed dose and resume your regular schedule.
Storage: Store unused Ozempic pens in the refrigerator (2°C to 8°C). Once in use, the pen can be kept at room temperature (below 30°C) or in the refrigerator for up to six weeks. Protect from light and do not freeze.
Drug interactions: Inform your healthcare provider about all medications you take. Ozempic may delay gastric emptying, potentially affecting the absorption of oral medications. If you take warfarin or other coumarin anticoagulants, more frequent INR monitoring is recommended when initiating Ozempic. Particular attention is needed if you take insulin or sulphonylureas, as dose adjustments may be necessary to prevent hypoglycaemia.
Insulin adjustments: Do not abruptly reduce or stop insulin when starting Ozempic, as this may increase the risk of diabetic ketoacidosis (DKA). Follow your clinician's guidance on any insulin dose adjustments.
Monitoring: Continue regular blood glucose monitoring as advised by your diabetes team. NICE guidance recommends monitoring HbA1c levels every 3–6 months to assess treatment effectiveness.
Pregnancy and breastfeeding: Ozempic is not recommended during pregnancy or breastfeeding. If you are planning pregnancy, discuss this with your doctor, as semaglutide should be discontinued at least two months before conception.
Age and diabetes type: Ozempic is not recommended for those under 18 years of age and is not indicated for type 1 diabetes or diabetic ketoacidosis.
Patient support: The NHS and Diabetes UK offer resources and support for people using injectable diabetes medications. Your GP practice or diabetes clinic can provide additional training, troubleshooting advice, and ongoing monitoring to ensure safe and effective treatment. If you experience persistent side effects or have concerns about your treatment, do not discontinue Ozempic without consulting your healthcare provider, as abrupt cessation may lead to deterioration in blood glucose control.
Yes, you can generally drink coffee and consume caffeine whilst taking Ozempic, as there is no official contraindication or direct pharmacological interaction between semaglutide and caffeine. However, if you experience nausea or gastrointestinal discomfort with Ozempic, reducing caffeine intake or consuming it with food may help minimise symptoms.
The sole active ingredient in Ozempic is semaglutide, a synthetic glucagon-like peptide-1 (GLP-1) receptor agonist that improves blood sugar control in adults with type 2 diabetes. The medication also contains inactive excipients such as disodium phosphate dihydrate, propylene glycol, phenol, and water for injections to maintain stability and sterility.
The most common side effects of Ozempic are nausea and diarrhoea, affecting more than 1 in 10 people, particularly during initial treatment or dose increases. Other common effects include vomiting, constipation, abdominal discomfort, and decreased appetite, which typically improve as the body adjusts to the medication.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.