
Many patients prescribed Ozempic for type 2 diabetes wonder about its composition and whether it contains hormones such as testosterone. Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist administered as a once-weekly injection to improve glycaemic control. It does not contain testosterone or any other sex hormones. The medication works by stimulating insulin secretion, suppressing glucagon release, and slowing gastric emptying. Understanding what Ozempic contains—and what it does not—is essential for informed decision-making about diabetes management. This article clarifies the composition of Ozempic, its metabolic effects, and important considerations before starting treatment.
Quick Answer: Ozempic does not contain testosterone or any other sex hormones; it contains only semaglutide, a synthetic GLP-1 receptor agonist.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists. Ozempic is administered as a once-weekly subcutaneous injection, starting at 0.25 mg for 4 weeks, then typically increasing to 0.5 mg, with further increases to 1.0 mg or 2.0 mg if needed for glycaemic control.
The primary mechanism of action involves several complementary effects on glucose regulation. Ozempic stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning it only promotes insulin release when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared to some other diabetes medications. Additionally, it suppresses the release of glucagon—a hormone that raises blood glucose—thereby preventing excessive glucose production by the liver.
Beyond glycaemic control, Ozempic slows gastric emptying, which prolongs the feeling of fullness after meals and contributes to reduced appetite. This effect has led to significant weight loss in many patients, which is why semaglutide (under the brand name Wegovy at a higher dose) has also been licensed for weight management in certain individuals with obesity or overweight with comorbidities.
It is important to note that Ozempic does not contain insulin, testosterone, or any other hormones beyond the synthetic GLP-1 analogue semaglutide itself. The medication is designed specifically to modulate glucose metabolism and appetite regulation through its action on GLP-1 receptors found in the pancreas, brain, and gastrointestinal tract.
Ozempic is not indicated for the treatment of type 1 diabetes or diabetic ketoacidosis.
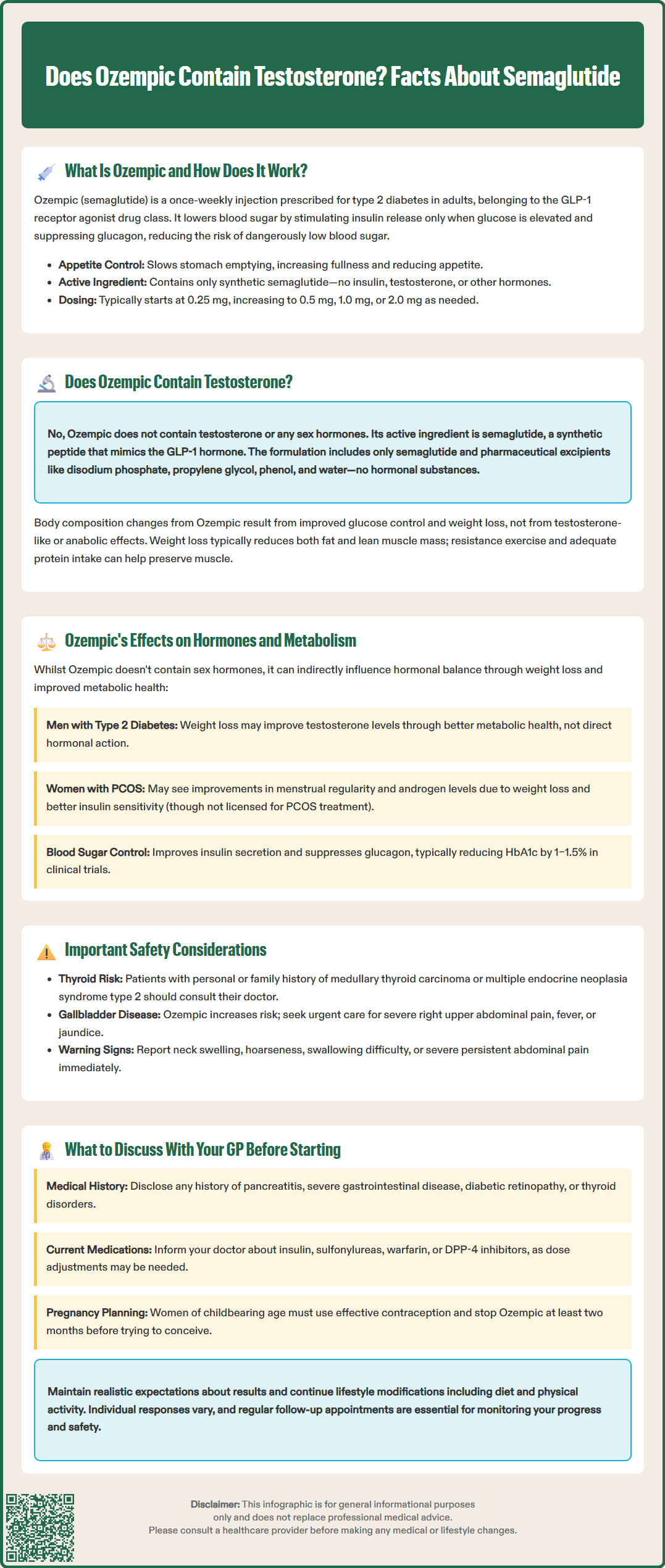
No, Ozempic does not contain testosterone. This is a common misconception that may arise from confusion about hormone-based therapies or the medication's effects on body composition and metabolism. Ozempic's active ingredient is semaglutide, a synthetic peptide that mimics the naturally occurring GLP-1 hormone. It contains no testosterone, oestrogen, growth hormone, or any other sex hormones or anabolic substances.
According to the UK Summary of Product Characteristics (SmPC), the formulation of Ozempic includes semaglutide along with pharmaceutical excipients such as disodium phosphate dihydrate, propylene glycol, phenol, and water for injections, as well as pH adjusters. None of these components are hormones, and the medication does not influence the body by introducing exogenous testosterone or other sex steroids.
Confusion may also stem from reports of metabolic changes or improvements in body composition that patients experience whilst taking Ozempic. However, these effects result from improved glucose control, reduced caloric intake, and weight loss—not from any testosterone-like or anabolic activity. It's worth noting that weight loss with GLP-1 receptor agonists typically reduces both fat and lean body mass. Patients concerned about preserving muscle mass during weight loss may benefit from resistance exercise and adequate protein intake.
If you have concerns about hormone levels—whether related to testosterone, thyroid function, or reproductive hormones—it is essential to discuss these separately with your GP. Certain individuals with type 2 diabetes may have coexisting hormonal imbalances (such as low testosterone in men or polycystic ovary syndrome in women), but these are independent conditions that require specific investigation and management. Ozempic does not treat or replace hormone deficiencies, nor does it contain any hormonal substances beyond its GLP-1 receptor agonist activity.
Whilst Ozempic does not contain testosterone or other sex hormones, it does exert significant effects on metabolic and hormonal pathways, primarily through its action on the GLP-1 receptor system. Understanding these effects is important for patients and healthcare professionals managing type 2 diabetes and associated metabolic conditions.
Insulin and glucagon regulation are the most direct hormonal effects. By enhancing glucose-dependent insulin secretion and suppressing inappropriate glucagon release, Ozempic helps restore a more physiological balance of these key metabolic hormones. This leads to improved glycaemic control, often reflected in reductions in HbA1c of 1–1.5% (approximately 11–16 mmol/mol) or more in clinical trials.
Weight loss associated with Ozempic can have secondary effects on various hormonal systems. In individuals with obesity, significant weight reduction may improve insulin sensitivity, reduce inflammatory markers, and positively influence sex hormone levels. For example, men with obesity and type 2 diabetes often have lower testosterone levels; weight loss may contribute to modest improvements in testosterone, though this is an indirect effect of metabolic improvement rather than a direct action of the drug.
Similarly, women with polycystic ovary syndrome (PCOS) and insulin resistance may experience improvements in menstrual regularity and androgen levels with weight loss, although Ozempic is not specifically licensed for PCOS treatment. Any such benefits would be secondary to improved insulin sensitivity and weight reduction.
Thyroid considerations are also relevant. The UK SmPC for Ozempic includes a precaution regarding thyroid C-cell tumours observed in rodent studies. Whilst there is no established link in humans, patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2 should discuss this with their healthcare provider. Routine calcitonin monitoring or thyroid ultrasound is not recommended, but patients should report any neck swelling, hoarseness, or difficulty swallowing to their GP promptly.
Patients should also be aware that GLP-1 receptor agonists, including Ozempic, are associated with an increased risk of gallbladder disease, including cholelithiasis and cholecystitis. Symptoms such as severe right upper abdominal pain, fever, or jaundice should prompt urgent medical attention.
Before initiating Ozempic, a thorough discussion with your GP or diabetes specialist is essential to ensure the medication is appropriate and safe for you. NICE guidance (NG28) recommends GLP-1 receptor agonists like Ozempic as a treatment option for type 2 diabetes in specific circumstances, such as part of triple therapy when BMI is ≥35 kg/m² (or lower in certain ethnic groups), when weight loss would benefit obesity-related comorbidities, or when insulin would be the next option but is not acceptable.
Key topics to discuss include:
Your complete medical history, particularly any history of pancreatitis (inflammation of the pancreas), severe gastrointestinal disease, diabetic retinopathy, or thyroid disorders. People with pre-existing diabetic retinopathy should be monitored closely, especially if rapid improvements in blood glucose control occur.
Current medications, as Ozempic may interact with certain drugs. Particular caution is needed if you take insulin or sulfonylureas, as the combination may increase the risk of hypoglycaemia, and dose adjustments may be necessary. If you take warfarin or other coumarin anticoagulants, your INR should be monitored when starting Ozempic. Combining GLP-1 receptor agonists with DPP-4 inhibitors is not recommended.
Kidney function, as while no dose adjustment is required for renal impairment, there is limited experience in end-stage renal disease. Your GP should monitor your renal function if you develop significant gastrointestinal side effects that could lead to dehydration.
Pregnancy and breastfeeding: Ozempic is not recommended during pregnancy or whilst breastfeeding. Women of childbearing potential should use effective contraception, and the medication should be discontinued at least two months before a planned pregnancy.
Realistic expectations regarding weight loss and glycaemic control. Whilst many patients experience significant benefits, individual responses vary. Your GP will discuss treatment targets and the importance of continuing lifestyle modifications, including diet and physical activity.
When to seek urgent medical attention whilst taking Ozempic includes: severe, persistent abdominal pain (which may indicate pancreatitis); signs of allergic reaction such as rash, swelling, or difficulty breathing; symptoms of thyroid masses; severe right upper abdominal pain, fever or jaundice (which may indicate gallbladder disease); or severe, persistent vomiting that could lead to dehydration. Regular follow-up appointments are essential to monitor treatment response, adjust doses, and assess for adverse effects.
If you experience any suspected side effects, report them to the MHRA through the Yellow Card scheme (yellowcard.mhra.gov.uk).
The active ingredient in Ozempic is semaglutide, a synthetic glucagon-like peptide-1 (GLP-1) receptor agonist. It does not contain testosterone, insulin, or any other hormones beyond the GLP-1 analogue.
Ozempic does not directly affect testosterone levels. However, weight loss achieved through Ozempic treatment may indirectly lead to modest improvements in testosterone levels in men with obesity and type 2 diabetes, as a result of improved metabolic health.
Ozempic is not suitable for people with type 1 diabetes, diabetic ketoacidosis, or a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2. It is also not recommended during pregnancy or breastfeeding.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.