
Does Ozempic help with alcohol cravings? This question has gained attention following anecdotal reports from patients and emerging preclinical research. Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for treating type 2 diabetes mellitus. Whilst animal studies suggest GLP-1 medications may reduce alcohol-seeking behaviour, human evidence remains preliminary and largely observational. Ozempic is not licensed or indicated for managing alcohol cravings, and established treatments for alcohol use disorder remain the recommended first-line approach. This article examines the current evidence, safety considerations, and appropriate support pathways for individuals concerned about alcohol consumption.
Quick Answer: Ozempic (semaglutide) is not licensed for treating alcohol cravings, though preliminary animal studies and anecdotal reports suggest GLP-1 receptor agonists may reduce alcohol consumption.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a prescription medication licensed in the UK for the treatment of type 2 diabetes mellitus. It belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone called GLP-1. This hormone plays a crucial role in regulating blood glucose levels and appetite.
The mechanism of action of Ozempic involves several key processes. Firstly, it stimulates insulin secretion from the pancreas in a glucose-dependent manner, meaning insulin is released only when blood sugar levels are elevated. This helps to lower blood glucose without causing excessive hypoglycaemia. Secondly, it suppresses glucagon release, a hormone that raises blood sugar levels. Thirdly, Ozempic slows gastric emptying, which means food moves more slowly from the stomach into the small intestine, leading to prolonged feelings of fullness and reduced appetite.
Ozempic is administered as a once-weekly subcutaneous injection, typically starting at a low dose (0.25 mg) for initiation only, which is not therapeutic, and gradually increasing to therapeutic doses of 0.5 mg, 1 mg, or 2 mg, depending on individual response and tolerability. The medication has gained considerable attention not only for its glucose-lowering effects but also for its associated weight loss benefits, which occur as a secondary effect of reduced appetite and caloric intake.
In the UK, Ozempic is regulated by the Medicines and Healthcare products Regulatory Agency (MHRA) and is available on NHS prescription for eligible patients with type 2 diabetes who meet specific criteria outlined by the National Institute for Health and Care Excellence (NICE) in guideline NG28. It is important to note that Ozempic is not currently licensed in the UK for weight management alone, though a higher-dose formulation of semaglutide (Wegovy) has been approved for this indication. Ozempic is not indicated for patients with type 1 diabetes or for the treatment of diabetic ketoacidosis.
Regarding pregnancy and breastfeeding, Ozempic should be discontinued at least 2 months before a planned pregnancy, should not be used during pregnancy, and is not recommended during breastfeeding, as outlined in the MHRA Summary of Product Characteristics.
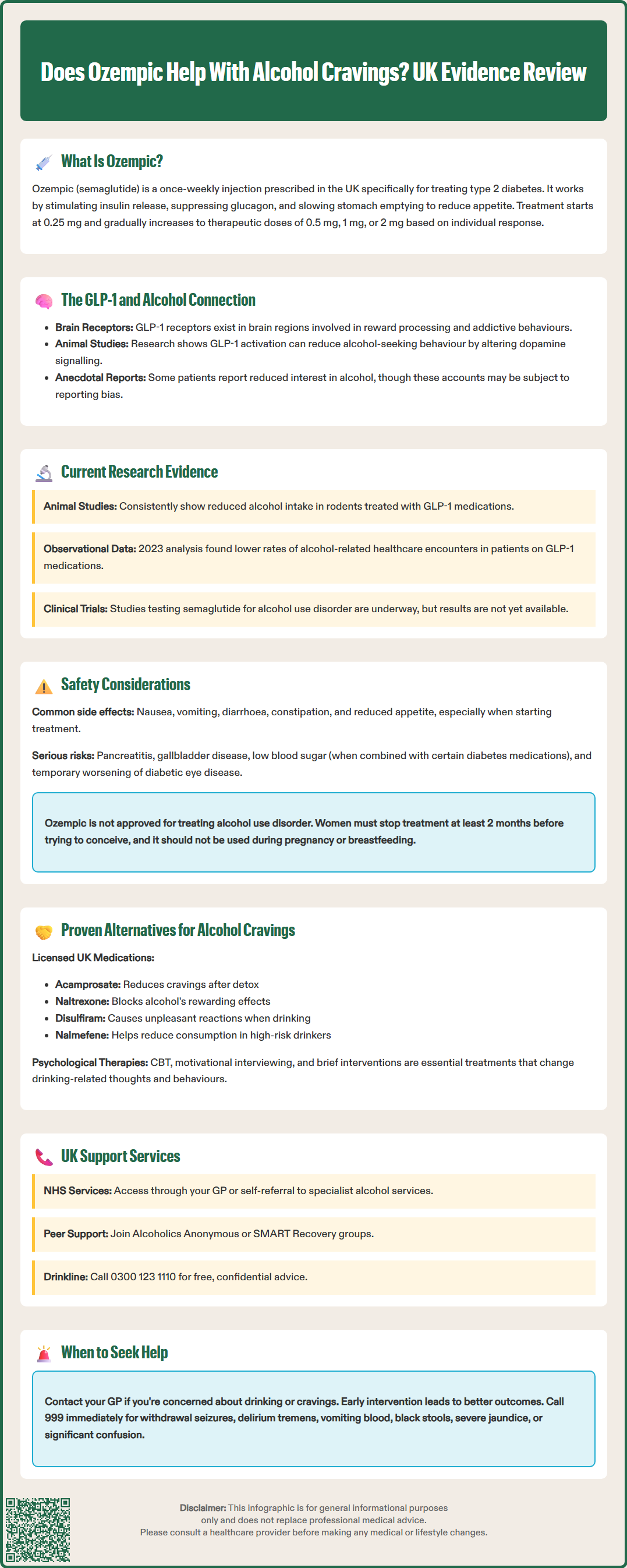
Recent scientific interest has emerged regarding the potential effects of GLP-1 receptor agonists on behaviours beyond glucose control and appetite regulation, including alcohol consumption and cravings. This interest stems from the discovery that GLP-1 receptors are present not only in the pancreas and gastrointestinal tract but also in various regions of the brain, particularly areas involved in reward processing and addictive behaviours.
The neurobiological basis for this connection lies in the mesolimbic dopamine system, often referred to as the brain's reward pathway. This system plays a central role in reinforcing behaviours associated with pleasure and reward, including eating, social interaction, and substance use. GLP-1 receptors are found in key structures within this pathway, including the ventral tegmental area (VTA) and nucleus accumbens, which are critically involved in processing rewarding stimuli.
Preclinical studies in animal models have demonstrated that activation of GLP-1 receptors can reduce alcohol-seeking behaviour and decrease voluntary alcohol consumption. These findings suggest that GLP-1 signalling may modulate the rewarding properties of alcohol, potentially making it less appealing or satisfying. The proposed mechanism involves alterations in dopamine signalling and changes in how the brain processes reward-related information.
Anecdotal reports from patients taking Ozempic and similar medications have described reduced interest in alcohol and decreased cravings for alcoholic beverages. Some individuals have reported finding alcohol less enjoyable or experiencing earlier satiation when drinking. However, it is crucial to emphasise that there is no official indication for Ozempic in treating alcohol use disorder, and these observations remain largely anecdotal and subject to reporting bias. The medication is not licensed or recommended for managing alcohol cravings, and any such effects should be considered preliminary and requiring further investigation.
It is important to note that the evidence in humans is highly preliminary and heterogeneous. Any consideration of GLP-1 receptor agonists for alcohol-related issues should be confined to formal research settings or specialist services, and not pursued as off-label treatment in routine clinical practice.
The scientific evidence examining the relationship between semaglutide (Ozempic) and alcohol consumption is still in its early stages, with most robust data coming from preclinical animal studies rather than large-scale human clinical trials. Understanding the current state of research is essential for contextualising claims about Ozempic's potential effects on alcohol cravings.
Animal studies have provided the most compelling evidence to date. Research using rodent models has consistently shown that GLP-1 receptor agonists, including semaglutide, can reduce alcohol intake and preference. These studies have demonstrated that animals treated with GLP-1 medications show decreased motivation to seek alcohol and consume less when it is available. The effects appear to be specific to alcohol rather than representing a general reduction in all consummatory behaviours.
Human research remains limited but is expanding. Several observational studies and case reports have documented reduced alcohol consumption among patients prescribed GLP-1 receptor agonists for diabetes or weight management. A retrospective analysis of electronic health records published in 2023 suggested that individuals taking GLP-1 medications had lower rates of alcohol-related healthcare encounters compared to those on other diabetes medications. However, this type of observational data cannot establish causation and may be influenced by numerous confounding factors, including weight loss, comorbidity burden, and concomitant therapies.
Existing randomised controlled trials with other GLP-1 receptor agonists (such as exenatide) in alcohol use disorder have shown mixed results, highlighting the need for caution when extrapolating from preclinical data to clinical outcomes.
Clinical trials specifically designed to test semaglutide's efficacy in treating alcohol use disorder are currently underway, as registered on ClinicalTrials.gov. These trials will provide more definitive evidence regarding whether Ozempic can meaningfully reduce alcohol cravings and consumption in individuals with problematic drinking patterns. Until these results are available, any conclusions remain speculative.
It is important to note that individual responses vary considerably. Not all patients taking Ozempic report changes in their alcohol consumption, and the magnitude of any effect appears to differ substantially between individuals. Factors such as baseline drinking patterns, genetic variations, and concurrent medications may all influence outcomes. The generalisability of findings from populations with type 2 diabetes to those with alcohol use disorder without diabetes also remains unclear.
When considering Ozempic for any indication, understanding its safety profile and potential adverse effects is paramount. Like all medications, Ozempic carries risks that must be weighed against potential benefits, and patients should be fully informed before commencing treatment.
Common adverse effects of Ozempic include:
Gastrointestinal symptoms: Nausea, vomiting, diarrhoea, constipation, and abdominal pain are the most frequently reported side effects, particularly during dose escalation. These symptoms typically improve over time but can be troublesome initially.
Reduced appetite: While often desired for weight management, decreased appetite can occasionally lead to inadequate nutritional intake.
Injection site reactions: Mild redness, swelling, or discomfort at the injection site may occur.
Serious but less common risks include:
Pancreatitis: There have been reports of acute pancreatitis in patients taking GLP-1 receptor agonists. If pancreatitis is suspected, Ozempic should be discontinued immediately and patients should seek urgent medical assessment. If pancreatitis is confirmed, Ozempic should not be restarted.
Gallbladder disease: Rapid weight loss associated with Ozempic may increase the risk of gallstones and cholecystitis.
Hypoglycaemia: When used in combination with insulin or sulfonylureas, the risk of low blood sugar increases.
Diabetic retinopathy complications: Rapid improvement in glucose control may temporarily worsen diabetic eye disease in susceptible individuals.
Special populations and precautions:
Pregnancy and breastfeeding: Ozempic should be discontinued at least 2 months before a planned pregnancy. It should not be used during pregnancy or breastfeeding.
Renal impairment: Caution is advised in patients with renal impairment, particularly if dehydration occurs due to gastrointestinal side effects. Renal function should be monitored if significant vomiting or diarrhoea occurs.
Severe gastrointestinal disease: Ozempic should be used with caution in patients with severe gastrointestinal disease, including severe gastroparesis.
Drug interactions: Ozempic may affect the absorption of oral medications due to delayed gastric emptying. Patients taking warfarin should have more frequent INR monitoring when starting or adjusting Ozempic. Caution is advised with narrow therapeutic index drugs.
Specific considerations regarding alcohol use: There is currently no official guidance suggesting that Ozempic directly interacts with alcohol or that it should be used to manage alcohol cravings. Patients who consume alcohol should be aware that both alcohol and Ozempic can affect blood sugar levels. Alcohol can increase the risk of hypoglycaemia, particularly when combined with other diabetes medications.
When to contact your GP:
Severe or persistent abdominal pain
Signs of pancreatitis (pain radiating to the back, nausea, vomiting)
Signs of gallbladder problems (right upper abdominal pain, especially after eating)
Signs of severe dehydration from vomiting or diarrhoea
Unexplained changes in vision
Symptoms of hypoglycaemia (shakiness, confusion, sweating)
Patients should never alter their prescribed medication regimen without consulting their healthcare provider, and Ozempic should not be used off-label for managing alcohol cravings without appropriate medical supervision and monitoring.
Patients are encouraged to report any suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
For individuals seeking help with alcohol cravings and problematic drinking, there are several evidence-based treatments and support services available in the UK, all of which have established efficacy and safety profiles for this specific indication.
Pharmacological treatments licensed for alcohol use disorder include:
Acamprosate (Campral): Helps restore the balance of neurotransmitters in the brain and reduces cravings. It is typically used to support abstinence after detoxification.
Naltrexone: An opioid receptor antagonist that reduces the rewarding effects of alcohol and can help decrease heavy drinking. Contraindicated in patients taking opioid medications and those with acute hepatitis or liver failure. Baseline liver function tests should be performed before starting treatment.
Disulfiram (Antabuse): Creates unpleasant reactions when alcohol is consumed, acting as a deterrent to drinking. Requires supervision and is contraindicated in certain cardiovascular conditions, pregnancy, and severe mental illness. Patients should be warned about the alcohol-disulfiram reaction.
Nalmefene: Used for reducing alcohol consumption in people with high-risk drinking levels who do not require immediate detoxification. According to NICE Technology Appraisal 325, it should only be prescribed alongside continuous psychosocial support focused on treatment adherence and reducing alcohol consumption.
These medications are recommended by NICE guidelines (CG115) for specific patient groups and should be prescribed as part of a comprehensive treatment programme.
Psychological interventions form the cornerstone of alcohol treatment:
Cognitive behavioural therapy (CBT): Helps identify and change thought patterns and behaviours related to drinking.
Motivational interviewing: A collaborative approach to strengthen motivation for change.
Brief interventions: Short, structured conversations that can be delivered in primary care settings, often using validated screening tools such as AUDIT-C or AUDIT.
Support services and resources available in the UK:
NHS alcohol support services: Available through GP referral or self-referral in many areas.
Alcoholics Anonymous (AA): Peer-led support groups following a 12-step programme.
SMART Recovery: An alternative mutual aid programme using cognitive-behavioural techniques.
Drinkline: A free, confidential helpline (0300 123 1110) providing advice and support.
Local alcohol treatment services: Specialist community services offering assessment, counselling, and structured treatment programmes.
When to seek help: If you are concerned about your alcohol consumption, experiencing cravings, or finding it difficult to control your drinking, contact your GP. They can assess your situation, provide initial advice, and refer you to specialist services if appropriate. Early intervention is associated with better outcomes, and seeking help is a sign of strength, not weakness.
Red flags requiring urgent medical attention include:
Alcohol withdrawal seizures
Delirium tremens (confusion, shaking, hallucinations)
Vomiting blood or passing black stools
Severe jaundice (yellowing of skin/eyes)
Significant confusion or reduced consciousness
If experiencing these symptoms, seek immediate emergency care via A&E or call 999.
It is important to emphasise that whilst emerging research on GLP-1 medications and alcohol cravings is intriguing, established treatments with proven efficacy should remain the first-line approach for managing alcohol use disorder. Any consideration of novel or off-label treatments should only occur within the context of specialist care and ongoing research protocols.
No, Ozempic is not licensed or approved in the UK for treating alcohol cravings or alcohol use disorder. It is only licensed for type 2 diabetes mellitus treatment, and any effects on alcohol consumption remain investigational.
Evidence is limited to animal studies showing reduced alcohol-seeking behaviour and observational human data. Randomised controlled trials specifically testing semaglutide for alcohol use disorder are currently underway but results are not yet available.
NICE-recommended treatments include medications such as acamprosate, naltrexone, disulfiram, and nalmefene, alongside psychological interventions like cognitive behavioural therapy and motivational interviewing. These should be accessed through your GP or specialist NHS alcohol services.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.