Ozempic (semaglutide) is a widely prescribed GLP-1 receptor agonist for type 2 diabetes management in the UK. As more patients use this once-weekly injection, questions arise about its effects beyond blood glucose control—including potential impacts on thyroid function. Specifically, some individuals wonder: does Ozempic lower TSH (thyroid-stimulating hormone)? Understanding the relationship between this diabetes medication and thyroid parameters is important for safe, informed treatment. This article examines current evidence, clarifies when thyroid monitoring may be appropriate, and provides guidance on discussing any concerns with your GP.
Quick Answer: There is no established causal link between Ozempic (semaglutide) and clinically significant reductions in TSH levels in the general population.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone that helps regulate blood sugar levels.
The mechanism of action involves several complementary effects. Ozempic stimulates insulin secretion from the pancreas when blood glucose levels are elevated, whilst simultaneously suppressing the release of glucagon, a hormone that raises blood sugar. Additionally, it slows gastric emptying, which means food moves more gradually from the stomach into the small intestine, helping to prevent sharp rises in blood glucose after meals. Many patients also experience reduced appetite and food intake, which can contribute to weight loss—a beneficial effect for many individuals with type 2 diabetes.
Ozempic is administered as a once-weekly subcutaneous injection, typically starting at a low dose (0.25 mg) for the first 4 weeks as an initiation dose only, and then increasing to therapeutic maintenance doses of 0.5 mg, 1 mg, or 2 mg, depending on individual response and tolerability. The MHRA has approved semaglutide specifically for glycaemic control in type 2 diabetes, and NICE guidelines (NG28) recommend GLP-1 receptor agonists as part of a comprehensive treatment strategy that includes lifestyle modifications.
It is important to note that whilst Ozempic has gained attention for weight loss effects, its primary indication remains diabetes management. For weight management specifically, a different semaglutide product called Wegovy is licensed in the UK. Patients should only use Ozempic under proper medical supervision, with regular monitoring to assess both efficacy and potential adverse effects.
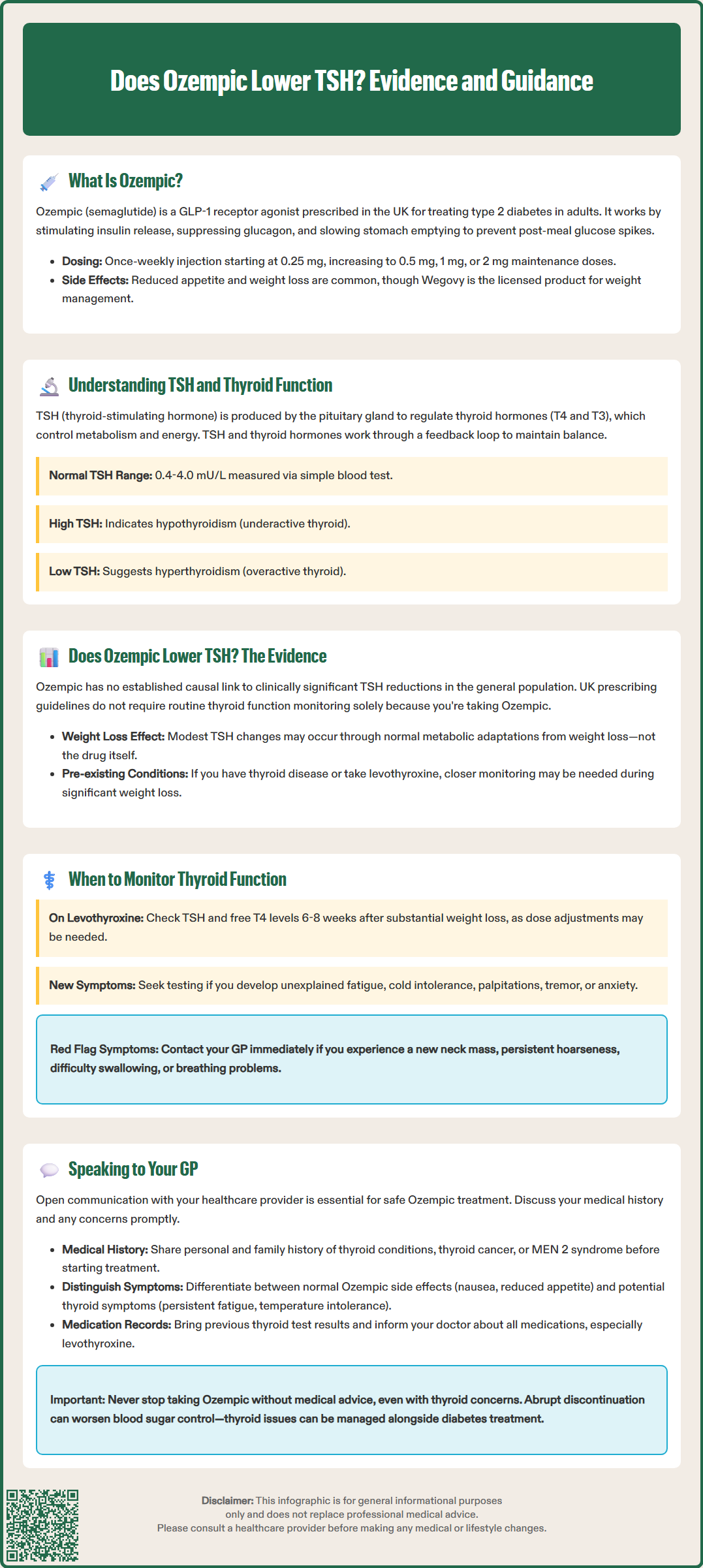
Thyroid-stimulating hormone (TSH) is a crucial hormone produced by the pituitary gland in the brain. Its primary role is to regulate the thyroid gland's production of thyroid hormones—thyroxine (T4) and triiodothyronine (T3)—which control metabolism, energy production, and numerous bodily functions.
The relationship between TSH and thyroid hormones operates through a negative feedback loop. When thyroid hormone levels in the blood are low, the pituitary releases more TSH to stimulate the thyroid gland to produce more hormones. Conversely, when thyroid hormone levels are adequate or elevated, TSH production decreases. This delicate balance ensures metabolic stability. An important exception is central hypothyroidism, where pituitary dysfunction can result in inappropriately low or normal TSH despite low thyroid hormone levels.
TSH levels are measured through a simple blood test and serve as the primary screening tool for thyroid dysfunction. Normal TSH ranges typically fall between 0.4 and 4.0 mU/L, though reference ranges vary between laboratories, with age, and during pregnancy. Elevated TSH usually indicates hypothyroidism (underactive thyroid), where the pituitary is working harder to stimulate an underperforming thyroid gland. Conversely, suppressed TSH often suggests hyperthyroidism (overactive thyroid), where excessive thyroid hormone production signals the pituitary to reduce TSH output.
Various factors can influence thyroid function, including autoimmune conditions (such as Hashimoto's thyroiditis or Graves' disease), iodine deficiency, certain medications, and thyroid nodules or cancer. Additionally, some medications—including lithium, amiodarone, and certain immunotherapy agents—are known to affect thyroid function. Understanding these interactions is essential when starting new treatments, particularly in patients with pre-existing thyroid conditions or risk factors.
The question of whether Ozempic directly lowers TSH levels requires careful examination of available clinical evidence. There is no established causal link between semaglutide and clinically significant reductions in TSH in the general population using the medication for type 2 diabetes management.
An important consideration exists for patients with a specific medical history. The Summary of Product Characteristics (SmPC) for Ozempic, as approved by the MHRA and EMA, notes that rodent studies showed thyroid C-cell tumours at high doses of semaglutide. However, the human relevance of these findings is uncertain. Unlike in the US, the UK and European SmPC does not contraindicate Ozempic in patients with a personal or family history of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia syndrome type 2 (MEN 2), but clinical vigilance is advised.
Limited data from case reports and observational studies suggest any effects of GLP-1 receptor agonists on thyroid function are typically small or potentially confounded by other factors. The EMA's European Public Assessment Report (EPAR) for Ozempic does not identify TSH suppression as a significant safety concern based on clinical trial data. Routine calcitonin or thyroid function monitoring is not required solely due to Ozempic use, according to the UK SmPC.
Weight loss itself—a common effect of Ozempic treatment—can influence thyroid hormone metabolism and TSH levels in complex ways. Significant weight reduction may lead to metabolic adaptations that affect thyroid function tests, though these changes are typically modest and not clinically concerning. If you have pre-existing thyroid disease or are taking levothyroxine, your healthcare team may monitor thyroid function more closely during significant weight changes, regardless of the method used to achieve weight loss.
Patients should be aware of red flags that warrant prompt GP assessment, including new neck lumps, persistent hoarseness, difficulty swallowing, or unexplained neck pain or swelling.
Routine thyroid function monitoring is not required for most patients starting or continuing Ozempic treatment. However, certain clinical scenarios warrant closer attention to thyroid parameters.
Patients with pre-existing thyroid conditions—such as hypothyroidism or hyperthyroidism—should continue their usual monitoring schedule as recommended by their GP or endocrinologist. If you are taking levothyroxine for hypothyroidism, your dose requirements may need adjustment if you experience significant weight loss on Ozempic, as body weight influences thyroid hormone replacement needs. Consider checking TSH and free T4 levels 6-8 weeks after substantial weight change or levothyroxine dose adjustment. Your healthcare provider will typically check TSH levels periodically to ensure your levothyroxine dose remains appropriate.
Additionally, monitoring may be considered if you develop symptoms suggestive of thyroid dysfunction whilst taking Ozempic. Signs of hypothyroidism include unexplained fatigue, cold intolerance, constipation, dry skin, and weight gain (though weight gain would be unusual on Ozempic). Symptoms of hyperthyroidism include palpitations, heat intolerance, tremor, anxiety, and unexplained weight loss beyond what would be expected from the medication's effects.
In line with NICE guidance (NG145), consider further investigation or referral if TSH is persistently above 10 mU/L or below 0.1 mU/L, or if free T4 or free T3 levels are abnormal. Red flags warranting prompt GP review include a new neck mass, persistent hoarseness, difficulty swallowing (dysphagia), or breathing difficulties (dyspnoea).
It is worth noting that some symptoms of thyroid dysfunction overlap with common side effects of GLP-1 receptor agonists. For example, gastrointestinal symptoms such as nausea and changes in bowel habits are frequent with Ozempic and do not necessarily indicate thyroid problems. Similarly, fatigue could relate to dietary changes, blood sugar fluctuations, or other factors rather than thyroid dysfunction.
NICE guidance on diabetes management (NG28) does not mandate routine thyroid screening specifically for patients on GLP-1 receptor agonists, but it does recommend that healthcare professionals remain vigilant for symptoms and consider thyroid function testing when clinically indicated. If you have concerns about thyroid-related symptoms, discuss them with your GP rather than discontinuing medication without medical advice.
If you have questions or concerns about Ozempic and thyroid function, open communication with your GP or diabetes specialist nurse is essential. Prepare for your appointment by noting any symptoms you have experienced, their duration and severity, and any relevant family history of thyroid disease.
Key points to discuss include:
Your personal and family medical history, particularly any thyroid conditions, thyroid cancer, or MEN 2 syndrome. While not a contraindication in the UK (unlike in the US), any history of medullary thyroid carcinoma should be discussed with your prescriber, as clinical vigilance is advised.
Current symptoms that concern you, distinguishing between expected medication side effects (such as nausea or reduced appetite) and potential thyroid-related symptoms (such as persistent fatigue, temperature intolerance, or palpitations).
Previous thyroid function tests, if available. Bring records of any historical TSH, T4, or T3 results, especially if you have known thyroid disease.
Other medications you are taking, including levothyroxine, as interactions and dose adjustments may be necessary.
Your GP can arrange appropriate investigations if clinically indicated. A thyroid function test typically includes TSH and free T4 measurements and requires a simple blood sample. Results are usually available within a few days. If abnormalities are detected, your GP will discuss whether they are clinically significant and require intervention, or whether they represent minor fluctuations that can be monitored.
Seek urgent GP assessment if you develop red flags such as a new or enlarging neck lump, persistent hoarseness, difficulty swallowing, or unexplained neck pain or swelling, as these may require referral under the NICE suspected cancer pathway (NG12).
Do not stop taking Ozempic without medical advice, even if you are concerned about thyroid effects. Abrupt discontinuation can lead to deterioration in blood glucose control. If thyroid dysfunction is confirmed, your healthcare team can manage both conditions concurrently—adjusting thyroid medication if needed whilst continuing diabetes treatment. Remember that the benefits of good glycaemic control in type 2 diabetes are substantial, reducing risks of cardiovascular disease, kidney disease, and other complications.
If you experience any suspected side effects from Ozempic, these can be reported through the MHRA Yellow Card Scheme, which helps monitor medication safety.
Routine thyroid function testing is not required before starting Ozempic unless you have pre-existing thyroid disease or relevant symptoms. Discuss your personal and family medical history with your GP, particularly any history of thyroid conditions or medullary thyroid carcinoma.
Significant weight loss from Ozempic may influence thyroid hormone replacement needs, potentially requiring levothyroxine dose adjustments. Your GP should monitor TSH and free T4 levels 6–8 weeks after substantial weight change to ensure your dose remains appropriate.
Seek prompt GP assessment if you develop a new neck lump, persistent hoarseness, difficulty swallowing, unexplained neck pain or swelling, or symptoms of thyroid dysfunction such as severe fatigue, palpitations, or temperature intolerance that cannot be explained by expected medication effects.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.