Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for treating type 2 diabetes mellitus. Whilst low energy on Ozempic is not listed as a common adverse reaction in the UK Summary of Product Characteristics, some patients report experiencing fatigue during treatment. This tiredness may relate to reduced caloric intake, gastrointestinal side effects, or metabolic adaptation. Understanding the causes, prevalence, and management strategies for low energy can help patients and clinicians optimise treatment outcomes whilst maintaining quality of life. This article examines the evidence, practical management approaches, and when to seek medical advice regarding fatigue during Ozempic therapy.
Quick Answer: Low energy on Ozempic may occur due to reduced caloric intake, gastrointestinal side effects, or metabolic adaptation, though fatigue is not listed as a common adverse reaction in UK prescribing information.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Fatigue is not listed as a common or very common adverse reaction in the UK Ozempic Summary of Product Characteristics (SmPC); however, some patients report experiencing low energy during treatment. Interestingly, fatigue is listed as common with higher-dose semaglutide for weight management (Wegovy).
Several plausible mechanisms may contribute to tiredness in some patients. The primary action involves slowing gastric emptying and reducing appetite, which leads to decreased caloric intake. When patients consume significantly fewer calories than their body requires, particularly during the initial weeks of treatment, this energy deficit may potentially manifest as tiredness or lethargy. Additionally, rapid weight loss—a common outcome of GLP-1 therapy—might temporarily affect energy levels as the body adapts to metabolic changes.
Gastrointestinal side effects such as nausea, vomiting, and reduced food intake are well-documented with Ozempic and may indirectly contribute to fatigue. If patients are unable to maintain adequate nutrition or hydration due to these symptoms, feelings of weakness and low energy may develop. Some patients may also experience temporary adjustment as their body acclimatises to more stable blood glucose levels after periods of hyperglycaemia.
It is important to consider alternative causes of fatigue, including anaemia, thyroid dysfunction, or other concurrent medical conditions, particularly if symptoms are severe or persistent. Clinicians should conduct appropriate investigations rather than automatically attributing fatigue to Ozempic treatment.
Sources: MHRA/EMC SmPC for Ozempic and Wegovy; EMA European Public Assessment Report (EPAR) for Ozempic
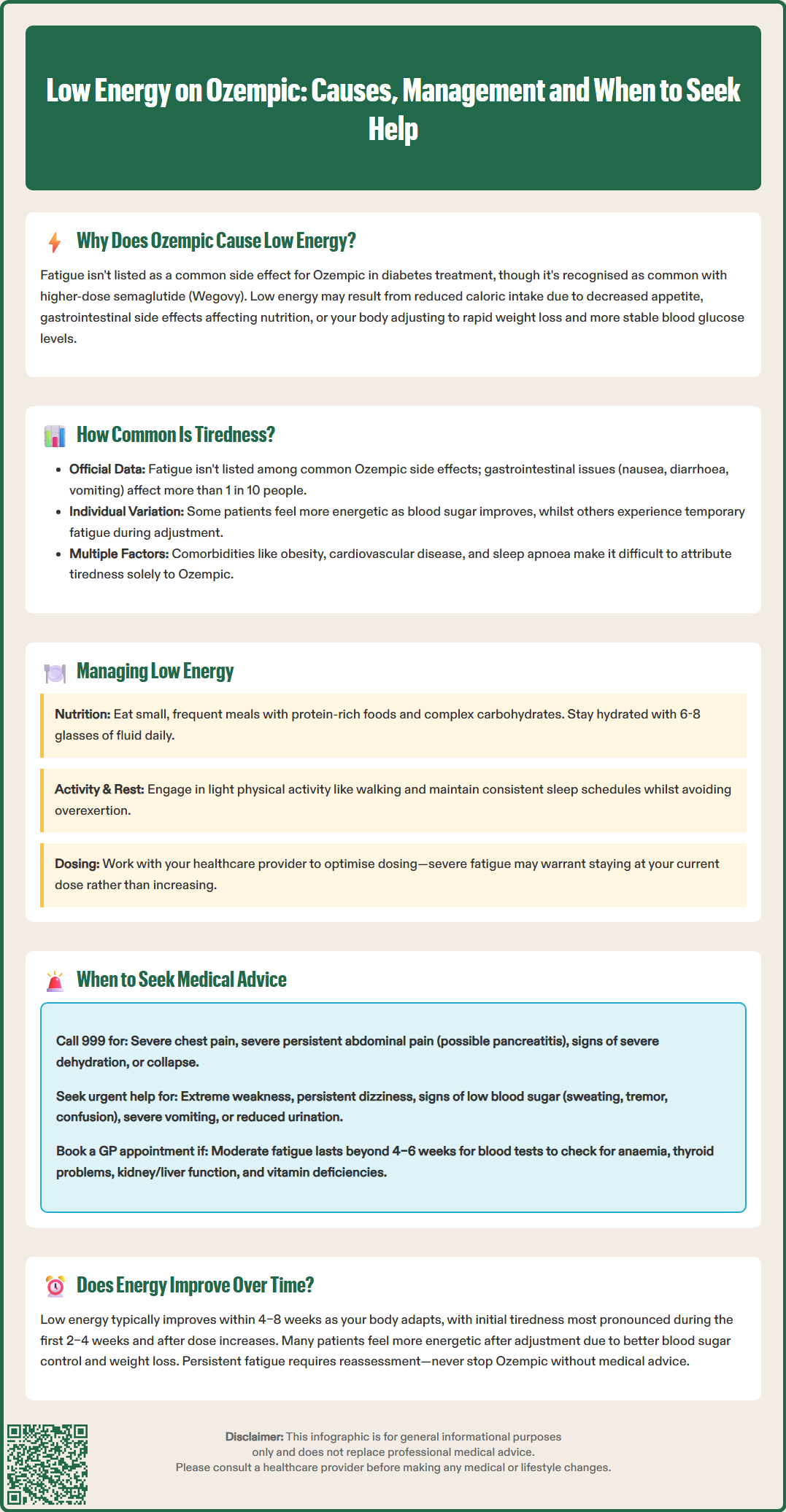
In the UK Ozempic SmPC, fatigue is not listed as common or very common; if reported, its frequency may be uncommon, rare or not known. Robust prevalence estimates are lacking. The most frequently reported side effects are gastrointestinal in nature, including nausea (occurring in more than 1 in 10 people), diarrhoea, vomiting, and constipation.
It is worth noting that fatigue is reported as common in Wegovy (higher-dose semaglutide for weight management), which may explain differing perceptions across indications and patient experiences.
The prevalence of low energy may be difficult to quantify because fatigue can be multifactorial and challenging to attribute solely to medication. Patients with type 2 diabetes often have multiple comorbidities—such as obesity, cardiovascular disease, or sleep apnoea—that independently contribute to tiredness. Additionally, lifestyle factors including dietary changes, increased physical activity, or psychological stress related to managing a chronic condition may influence energy levels.
Individual variation in response to GLP-1 receptor agonists is considerable. Some patients report feeling more energetic as their blood glucose control improves and excess weight is lost, whilst others experience temporary fatigue during the adjustment period. The dose escalation schedule recommended for Ozempic (starting at 0.25 mg weekly and increasing gradually) is designed to minimise side effects, but tolerance varies between individuals.
Patients taking Ozempic alongside insulin or sulphonylureas require particular monitoring, as the combination increases hypoglycaemia risk, which can manifest as fatigue.
Clinicians should acknowledge patient concerns about fatigue and conduct appropriate investigations to exclude other causes. Monitoring and supportive management can help patients continue treatment whilst addressing energy-related concerns effectively.
Sources: MHRA/EMC SmPC for Ozempic and Wegovy; NICE NG28: Type 2 diabetes in adults
Effective management of low energy during Ozempic treatment requires a multifaceted approach addressing nutrition, hydration, lifestyle factors, and potential underlying causes. Patients should be encouraged to maintain adequate caloric intake despite reduced appetite, focusing on nutrient-dense foods that provide sustained energy throughout the day.
Nutritional strategies include:
Consuming small, frequent meals rather than large portions to manage nausea whilst ensuring sufficient energy intake
Prioritising protein-rich foods (lean meat, fish, eggs, pulses) to support muscle mass during weight loss
Including complex carbohydrates (whole grains, vegetables) for sustained glucose release
Ensuring adequate hydration—aim for 6–8 glasses of fluid daily, as dehydration can exacerbate fatigue
Vitamin and mineral supplementation should only be considered if clinically indicated or advised by a healthcare professional following appropriate testing (e.g., ferritin/iron studies; vitamin B12 especially if on long-term metformin)
Lifestyle modifications can significantly impact energy levels. Regular physical activity, even light walking, can paradoxically improve fatigue by enhancing cardiovascular fitness and mood. However, patients should avoid overexertion during the adjustment period and gradually increase activity levels as tolerated. Sleep hygiene is equally important—maintaining consistent sleep schedules and addressing any sleep disturbances can help combat daytime tiredness.
Patients should work closely with their diabetes specialist nurse or GP to optimise their treatment regimen. If fatigue is severe, temporarily maintaining the current dose rather than escalating may be considered. Ozempic can be administered at any time of day; changing timing is a patient-preference strategy without strong evidence and should be guided by clinician advice.
For patients taking insulin or sulphonylureas alongside Ozempic, medication doses may need adjustment to reduce hypoglycaemia risk when appetite and caloric intake change. Regular monitoring of HbA1c and body weight can help assess whether treatment goals are being achieved whilst managing side effects appropriately.
Sources: NICE NG28: Type 2 diabetes in adults; NHS advice on hydration and healthy eating; MHRA/EMC SmPC for Ozempic
Whilst mild tiredness during the initial weeks of Ozempic treatment may be manageable with lifestyle adjustments, certain presentations warrant prompt medical evaluation. Patients should be advised to contact their GP or diabetes care team if fatigue is severe, persistent, or accompanied by other concerning symptoms.
Red flag symptoms requiring urgent assessment include:
Extreme weakness or inability to perform daily activities
Persistent dizziness, particularly on standing (which may indicate dehydration or hypotension)
Symptoms of hypoglycaemia—sweating, tremor, confusion, palpitations—especially in patients taking insulin or sulphonylureas concurrently
Chest pain, breathlessness, or palpitations suggesting cardiovascular complications
Severe or persistent vomiting leading to dehydration
Reduced urine output (a warning sign of dehydration or acute kidney injury)
Signs of pancreatitis: severe, persistent abdominal pain radiating to the back
Jaundice or dark urine, which may indicate hepatobiliary complications
For severe chest pain, severe persistent abdominal pain (possible pancreatitis), signs of severe dehydration or collapse, call 999 or attend A&E immediately. If unsure about the severity, contact NHS 111 for advice.
Patients experiencing moderate fatigue lasting beyond 4–6 weeks should arrange a routine appointment for clinical review. The GP should conduct a thorough assessment including physical examination and appropriate investigations. Blood tests may include full blood count (to exclude anaemia), renal and liver function, thyroid function tests, vitamin B12 and folate levels, and HbA1c to assess glycaemic control.
It is particularly important to evaluate for alternative causes of fatigue that may coincide with, but are not caused by, Ozempic treatment. These include hypothyroidism, anaemia, chronic kidney disease, depression, sleep disorders, or other endocrine abnormalities. If investigations reveal an underlying condition, appropriate treatment should be initiated.
Patients should never discontinue Ozempic without medical advice, as abrupt cessation may lead to deterioration in glycaemic control. If fatigue is intolerable despite supportive measures, the prescriber may consider dose adjustment, temporary treatment interruption, or switching to an alternative diabetes medication. Shared decision-making between patient and clinician is essential to balance treatment efficacy with quality of life considerations.
Sources: MHRA/EMC SmPC for Ozempic – pancreatitis and gallbladder disease warnings; NHS guidance on hypoglycaemia and when to seek urgent help
For many patients who experience low energy when starting Ozempic, symptoms typically improve within 4–8 weeks as the body adapts to the medication and its metabolic effects, though individual variation is substantial. This adjustment period often coincides with the dose escalation phase, during which gastrointestinal side effects also tend to diminish. As patients establish new eating patterns and their bodies adapt to reduced caloric intake, energy levels often stabilise or improve.
Based on clinical experience, the pattern of treatment-related fatigue may follow a predictable course for some patients. Initial tiredness may be most pronounced during the first 2–4 weeks, particularly after dose increases. As gastric emptying slows and appetite decreases, patients learn to adjust their dietary habits, consuming smaller, more frequent meals that maintain energy levels throughout the day. Concurrently, improvements in glycaemic control and progressive weight loss may lead to enhanced overall wellbeing, which can offset initial fatigue.
Some patients report feeling more energetic after the adjustment period compared to before starting treatment. This improvement may potentially result from better blood glucose control, weight loss benefits, and possibly improved sleep quality (particularly if weight reduction helps with sleep apnoea). These positive effects can outweigh any initial tiredness experienced during treatment initiation.
However, a proportion of patients may experience persistent fatigue that does not resolve over time. In such cases, it is crucial to reassess whether Ozempic is the appropriate treatment choice. Factors to consider include the degree of glycaemic improvement achieved, amount of weight lost, presence of other side effects, and impact on quality of life. Alternative GLP-1 receptor agonists or different classes of diabetes medications may be better tolerated in some individuals.
Long-term monitoring is essential to ensure that fatigue does not indicate an underlying complication or nutritional deficiency. Patients should maintain regular contact with their diabetes care team and report any persistent or worsening symptoms. With appropriate support and management, most patients can successfully adapt to Ozempic treatment and achieve their therapeutic goals whilst maintaining good energy levels and quality of life.
Patients are encouraged to report any suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Sources: EMA EPAR for Ozempic – tolerability over time; NICE NG28: Type 2 diabetes in adults; MHRA Yellow Card Scheme
For most patients, low energy typically improves within 4–8 weeks as the body adapts to Ozempic and its metabolic effects. If fatigue persists beyond this period, contact your GP for clinical review and appropriate investigations.
Maintain adequate caloric intake through small, frequent, nutrient-dense meals, ensure proper hydration (6–8 glasses daily), prioritise protein-rich foods, and engage in regular light physical activity. Work closely with your diabetes care team to optimise your treatment regimen.
Seek urgent medical attention for severe weakness, persistent vomiting, chest pain, severe abdominal pain, or signs of hypoglycaemia. Arrange a routine GP appointment if moderate fatigue persists beyond 4–6 weeks or is accompanied by other concerning symptoms.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.