
Discussing weight loss injections with your GP requires preparation and understanding of eligibility criteria. GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda) are prescription-only medicines regulated by the MHRA for obesity management in the UK. These treatments are available through the NHS for eligible patients meeting specific BMI thresholds and participating in specialist weight management services, or privately for those seeking faster access. This article guides you through understanding these medications, determining eligibility, preparing for your consultation, and navigating NHS versus private treatment pathways to help you have an informed, productive conversation with your healthcare provider about whether weight loss injections are appropriate for your individual circumstances.
Quick Answer: To ask your GP for weight loss injections, prepare by calculating your BMI, documenting previous weight loss attempts, and understanding NHS eligibility criteria (typically BMI ≥35 kg/m² or ≥30 kg/m² with comorbidities).
Weight loss injections, medically known as GLP-1 receptor agonists, have become an increasingly discussed treatment option for obesity management in the UK. The most commonly prescribed medications in this class include semaglutide (marketed as Wegovy for weight management) and liraglutide (Saxenda). These medications were originally developed for type 2 diabetes management but have demonstrated significant efficacy in weight reduction.
These injections work by mimicking a naturally occurring hormone called glucagon-like peptide-1 (GLP-1), which regulates appetite and food intake. The mechanism of action involves:
Enhancing glucose-dependent insulin secretion and reducing glucagon production
Slowing gastric emptying, which helps you feel fuller for longer periods
Reducing appetite by acting on brain receptors that control hunger
Decreasing food intake through these combined effects
These medications are administered by subcutaneous injection, with semaglutide given once weekly and liraglutide daily. Both require gradual dose titration to reach the therapeutic dose (2.4mg for semaglutide; 3.0mg for liraglutide).
It is important to understand that weight loss injections are not cosmetic treatments or quick fixes. They are prescription-only medicines regulated by the Medicines and Healthcare products Regulatory Agency (MHRA) and are intended as part of a comprehensive weight management programme. This programme typically includes dietary modifications, increased physical activity, and behavioural support.
Common side effects include nausea, vomiting, diarrhoea, constipation, and abdominal discomfort, particularly when starting treatment or increasing doses. Small increases in heart rate are common but usually not serious. More serious but rare adverse effects can include pancreatitis and gallbladder problems.
These medications require careful medical supervision and regular monitoring. Pregnancy is a contraindication, and caution is needed in certain conditions, including personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2. If you experience severe, persistent abdominal pain (with or without vomiting), seek urgent medical attention as this could indicate pancreatitis.
If you suspect any adverse reactions to these medications, report them through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk). Understanding these fundamentals will help you have an informed conversation with your healthcare provider about whether this treatment approach is appropriate for your individual circumstances.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereThe National Institute for Health and Care Excellence (NICE) provides clear guidance on eligibility criteria for weight loss injections through the NHS. These criteria are based on clinical evidence and cost-effectiveness considerations, ensuring that treatments are offered to those who will benefit most whilst managing limited NHS resources responsibly.
For semaglutide (Wegovy), NICE recommends prescription for adults who meet the following criteria:
A body mass index (BMI) of 35 kg/m² or above, or
A BMI of 30–34.9 kg/m² with at least one weight-related comorbidity such as hypertension, type 2 diabetes, obstructive sleep apnoea, or cardiovascular disease
Participation in a specialist weight management service that provides dietary advice, physical activity support, and behavioural interventions
Treatment duration should not exceed 2 years in NHS settings
For individuals from South Asian, Chinese, other Asian, Middle Eastern, Black African, or African-Caribbean backgrounds, BMI thresholds are 2.5 kg/m² lower due to increased metabolic risk at lower body weights. In these populations, treatment may be considered at BMI 32.5 kg/m² or above (or 27.5–32.4 kg/m² with comorbidities).
Liraglutide (Saxenda) has similar eligibility criteria, but with a different stopping rule: treatment should be discontinued if 5% weight loss is not achieved after 12 weeks at the maintenance dose of 3.0mg daily.
For semaglutide, treatment is typically discontinued if patients do not achieve at least 5% weight loss after 6 months of therapy, as continued use is unlikely to provide meaningful benefit.
While NICE technology appraisals should be implemented by the NHS, availability may be affected by service capacity and national supply constraints. Some areas have restricted access due to these practical challenges.
Weight loss injections are not suitable for everyone. Contraindications include pregnancy, and caution is needed in conditions such as history of pancreatitis, gallbladder disease, and severe gastrointestinal disorders. Your GP will assess your full medical history, current medications, and individual circumstances to determine eligibility.
It's important to have realistic expectations and understand that these medications are intended to support lifestyle changes, not replace them. The NHS pathway typically involves comprehensive support from healthcare professionals specialising in obesity management.
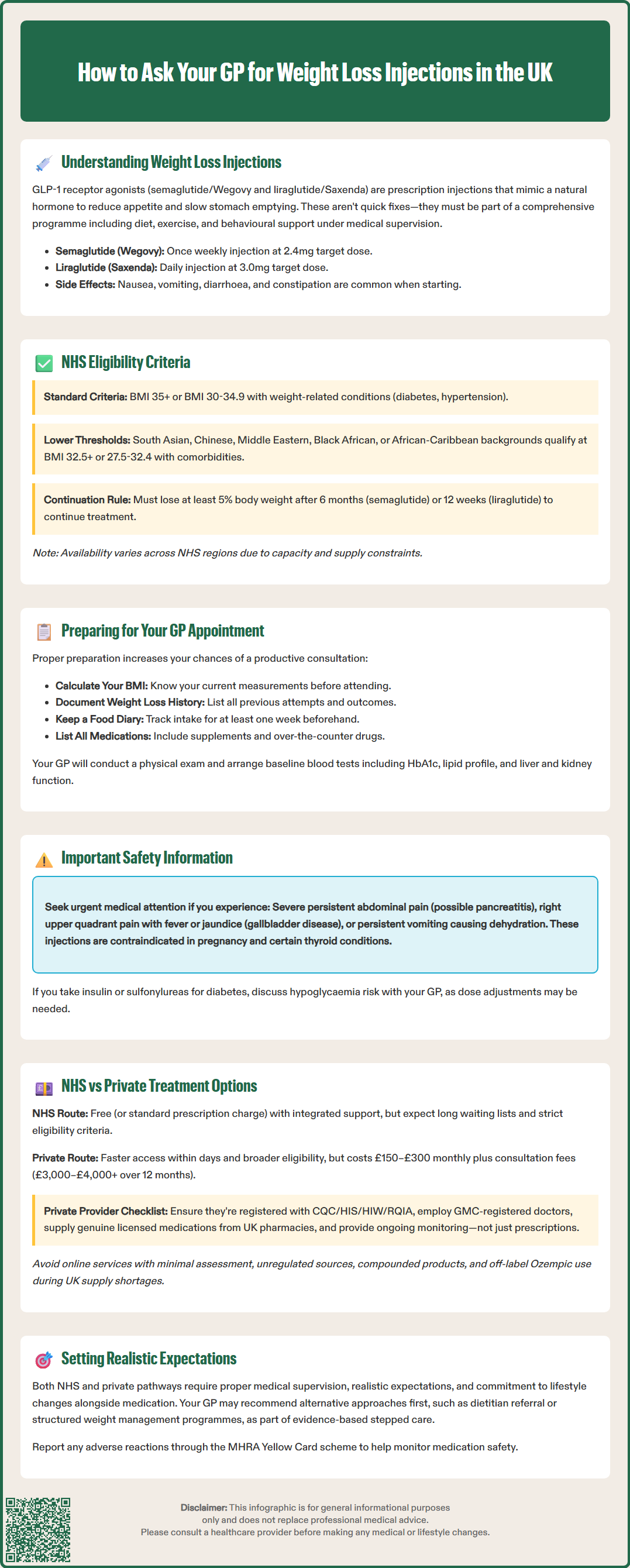
Approaching your GP about weight loss injections requires thoughtful preparation to ensure a productive consultation. Your doctor will need to assess whether this treatment is clinically appropriate, safe, and likely to be effective for your specific situation. Being well-prepared demonstrates your commitment to weight management and helps your GP make an informed decision.
Before your appointment, consider taking the following steps:
Calculate your BMI using your current height and weight, and track your weight history over recent months or years
Document previous weight loss attempts, including dietary changes, exercise programmes, commercial weight loss services, or other medical interventions you have tried
List all current medications and supplements, as some may interact with GLP-1 receptor agonists or affect weight
Note any weight-related health conditions such as type 2 diabetes, high blood pressure, high cholesterol, joint problems, sleep apnoea, or polycystic ovary syndrome
Keep a food and activity diary for at least one week to demonstrate your current lifestyle patterns
Prepare questions about the treatment, including administration technique, side effects, duration, and monitoring requirements
During the consultation, be honest and open about your weight management challenges, emotional relationship with food, and realistic expectations. Your GP will likely:
Conduct a physical examination and review your medical history
Discuss the risks and benefits of weight loss injections specific to your health profile
Explain the commitment required, including lifestyle modifications and regular follow-up appointments
Arrange baseline investigations which may include blood tests to check HbA1c, lipid profile, liver and kidney function, and thyroid function, though these will be tailored to your individual circumstances
Assess for contraindications or cautions such as pregnancy plans (contraception is recommended during treatment, with semaglutide requiring at least 2 months' washout before planned conception)
If you have diabetes and take insulin or sulfonylureas, discuss the potential increased risk of hypoglycaemia when adding GLP-1 receptor agonists. Similarly, as these medications delay gastric emptying, timing of certain critical oral medications may need adjustment.
Be aware of warning signs requiring urgent medical attention: severe persistent abdominal pain (which might indicate pancreatitis), right upper quadrant pain/fever/jaundice (gallbladder disease), or persistent vomiting causing dehydration.
Be prepared for the possibility that your GP may suggest alternative approaches first, such as referral to a dietitian, structured weight management programme, or psychological support for eating behaviours. This is not a rejection but reflects evidence-based stepped care. If you do not meet NHS eligibility criteria, your GP can discuss private treatment options or other evidence-based interventions. Remember that your GP is your partner in health management, and an open, collaborative conversation will yield the best outcomes.
Understanding the differences between NHS and private pathways for accessing weight loss injections is essential for making an informed decision that suits your circumstances, budget, and timeline. Both routes have distinct advantages and considerations.
NHS provision offers several benefits:
No direct cost for prescriptions (standard prescription charges apply in England; free in Scotland, Wales, and Northern Ireland)
Integrated care within specialist weight management services, including dietetic support, physical activity guidance, and psychological interventions
Ongoing monitoring and follow-up as part of comprehensive care
Evidence-based protocols following NICE guidance
However, NHS access faces significant challenges. Many areas have restricted or paused new prescriptions due to service capacity, budget pressures and medication supply constraints. Waiting lists for specialist weight management services can extend to several months or longer. Strict eligibility criteria mean many individuals who might benefit clinically do not qualify for NHS-funded treatment.
Private treatment offers alternative access:
Faster access without lengthy waiting lists, often with appointments available within days
Broader eligibility, with some private providers treating patients at lower BMI thresholds
Flexible appointment scheduling and potentially more consultation time
Choice of provider, including online services, private GPs, and specialist weight management clinics
The primary consideration is cost. Private prescriptions for semaglutide typically range from £150–£300 per month, with liraglutide similarly priced. Initial consultations, follow-up appointments, and monitoring investigations incur additional fees. Over a typical 12-month treatment course, total costs can exceed £3,000–£4,000.
Important safety considerations apply regardless of pathway. Ensure any private provider:
Is registered with the Care Quality Commission (CQC) in England, Healthcare Improvement Scotland (HIS), Healthcare Inspectorate Wales (HIW), or the Regulation and Quality Improvement Authority (RQIA) in Northern Ireland
Employs GMC-registered doctors who conduct proper medical assessments
Provides genuine licensed medications from regulated UK pharmacies, not unregulated imports or compounded products
Adheres to UK product licences and GMC prescribing standards
Offers ongoing monitoring and support, not just prescription provision
Has clear protocols for managing side effects and medical emergencies
Be cautious of online services offering prescriptions after minimal assessment, as these may not provide adequate medical oversight. Avoid purchasing from unregulated sources or using compounded products. Note that Ozempic (semaglutide 1mg) is not licensed for weight management in the UK, and the Department of Health and Social Care has advised against its off-label use during supply shortages.
Whether pursuing NHS or private treatment, your safety depends on proper medical supervision, realistic expectations, and commitment to comprehensive lifestyle changes alongside medication. Report any suspected side effects via the MHRA Yellow Card scheme. Discuss both options openly with your GP, who can provide guidance tailored to your individual health needs and circumstances.
You typically need a BMI of 35 kg/m² or above, or a BMI of 30–34.9 kg/m² with at least one weight-related condition such as type 2 diabetes or hypertension. For South Asian, Chinese, other Asian, Middle Eastern, Black African, or African-Caribbean backgrounds, thresholds are 2.5 kg/m² lower.
Calculate your BMI, document previous weight loss attempts, list all current medications, note weight-related health conditions, and keep a food and activity diary for at least one week. Prepare questions about administration, side effects, and monitoring requirements to demonstrate your commitment to treatment.
NHS treatment is provided at no direct cost (standard prescription charges apply in England) with integrated specialist support but faces waiting lists and strict eligibility criteria. Private treatment offers faster access and broader eligibility but costs £150–£300 monthly, with total costs potentially exceeding £3,000–£4,000 over 12 months.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.