
Discussing weight loss injections with your GP requires preparation and understanding of what these medications can realistically achieve. Weight loss injections, such as semaglutide (Wegovy) and liraglutide (Saxenda), are prescription-only GLP-1 receptor agonists licensed for adults with obesity or weight-related health conditions. They are not cosmetic treatments but medical interventions requiring ongoing commitment, lifestyle changes, and regular monitoring. NHS eligibility follows strict NICE criteria, typically requiring a BMI of 35 kg/m² or above with weight-related comorbidities, whilst private treatment offers faster access at significant cost. This guide helps you prepare for a productive conversation with your doctor, understand eligibility pathways, ask informed questions, and set realistic expectations about treatment outcomes and potential side effects.
Quick Answer: Prepare for your GP appointment by documenting your weight history, current medications, and weight-related health concerns, then ask specific questions about eligibility, medication options, administration, expected outcomes, and monitoring requirements.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections, medically termed anti-obesity medications (AOMs), have become an increasingly discussed treatment option for individuals struggling with obesity or weight-related health conditions. In the UK, the primary medications available include semaglutide (marketed as Wegovy) and liraglutide (marketed as Saxenda), both belonging to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists. Tirzepatide, a dual GIP/GLP-1 receptor agonist, is also emerging in the UK weight management landscape.
These medications work by mimicking naturally occurring hormones that regulate appetite and food intake. GLP-1 receptor agonists slow gastric emptying, increase feelings of fullness after eating, and reduce hunger signals in the brain. This mechanism helps patients consume fewer calories whilst feeling satisfied, leading to gradual, sustainable weight loss when combined with lifestyle modifications.
It's important to understand that weight loss injections are not cosmetic treatments or quick fixes. They are prescription-only medicines approved by the Medicines and Healthcare products Regulatory Agency (MHRA) for specific clinical indications. These medications are licensed for adults (18+ years) with a body mass index (BMI) of 30 kg/m² or above, or 27 kg/m² or above with at least one weight-related comorbidity such as type 2 diabetes, hypertension, or obstructive sleep apnoea. They should not be used during pregnancy or breastfeeding.
However, NHS-funded eligibility criteria are more restrictive than the licensed indications. NICE guidance typically recommends these treatments for people with higher BMI thresholds (generally 35 kg/m² or above, or 32.5 kg/m² for people from certain ethnic backgrounds) and requires treatment within specialist weight management services.
Before discussing these treatments with your doctor, familiarising yourself with how they work and their intended purpose will help you have a more informed conversation. Understanding that these injections require ongoing commitment, regular monitoring, and concurrent lifestyle changes sets realistic expectations from the outset. Your GP will assess whether you meet the clinical criteria and whether this treatment approach aligns with your overall health goals and medical history.
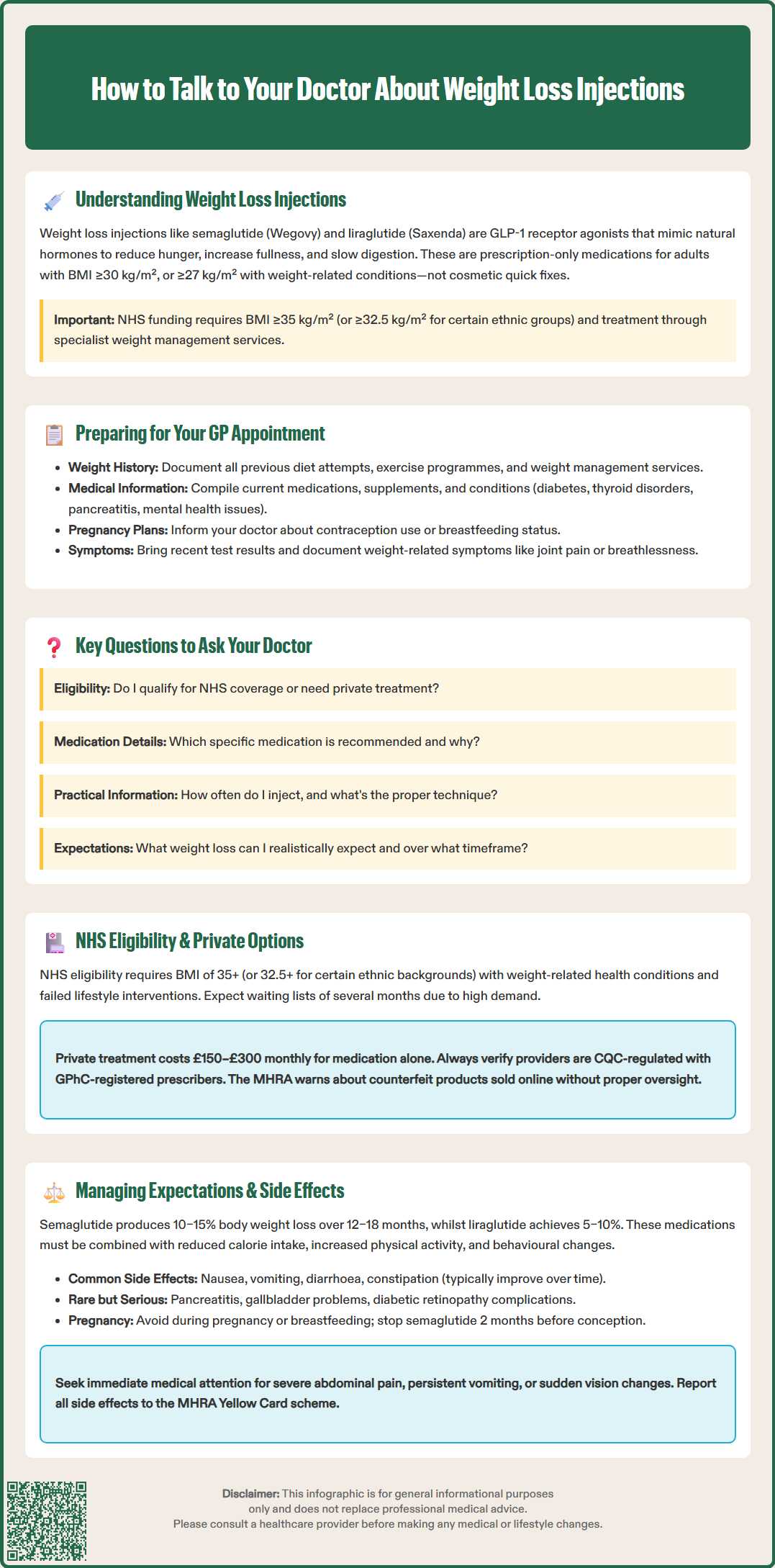
Adequate preparation before your appointment will ensure a productive discussion with your doctor about weight loss injections. Begin by documenting your weight history, including previous weight loss attempts, diets tried, exercise programmes undertaken, and any commercial weight management services you've accessed. This information helps your GP understand the extent of your efforts and whether you meet the criteria for medical intervention.
Compile a comprehensive list of your current medications, supplements, and herbal remedies. Certain medications may interact with GLP-1 receptor agonists, and some conditions may contraindicate their use. If you have diabetes and take insulin or sulfonylureas, be sure to bring details of your diabetes treatment, as dose adjustments may be needed to prevent hypoglycaemia. Include any history of thyroid disorders, pancreatitis, gallbladder disease, diabetic retinopathy, or mental health conditions, as these factors influence treatment decisions.
Be prepared to discuss your pregnancy plans, contraception use, or breastfeeding status, as weight loss injections are not suitable during pregnancy or breastfeeding and require effective contraception during treatment.
Prepare to discuss your weight-related health concerns honestly. Document any symptoms you experience that may be linked to excess weight, such as joint pain, breathlessness, sleep disturbances, or difficulties with daily activities. If you have conditions like type 2 diabetes, hypertension, or high cholesterol, bring recent test results or know your latest readings. If available, bring reports related to sleep apnoea or other weight-related conditions.
Consider writing down your specific questions and concerns beforehand. Appointments can feel rushed, and it's easy to forget important points during the consultation. Having a written list ensures you address everything that matters to you. Be prepared to discuss your lifestyle, including typical eating patterns, physical activity levels, work schedule, and any barriers you face in making healthy changes.
Finally, reflect on your motivations and readiness for change. Your doctor will want to understand why you're seeking treatment now and whether you're prepared to commit to the lifestyle modifications that must accompany medication. Demonstrating genuine commitment to comprehensive weight management increases the likelihood of a positive outcome from your consultation.
Asking informed questions during your consultation empowers you to make decisions about your treatment. Start by asking, "Am I eligible for weight loss injections on the NHS, or would I need to pursue private treatment?" Understanding the pathway available to you helps set realistic expectations regarding access and costs.
Inquire about which specific medication your doctor recommends and why. Ask, "What are the differences between semaglutide and liraglutide, and which would be most suitable for my situation?" Different medications have varying dosing schedules, efficacy profiles, and side effect patterns. Understanding these distinctions helps you participate actively in treatment selection.
Discuss the practical aspects of administration: "How often will I need to inject? Can you show me the proper injection technique? What areas of the body are suitable for injection? How should I rotate injection sites?" Most weight loss injections are administered subcutaneously (under the skin) once weekly or daily, depending on the medication. Ensuring you're comfortable with self-administration is crucial for adherence.
Ask about expected outcomes and treatment duration: "What amount of weight loss is realistic? How long does treatment typically continue? What happens if the medication doesn't work for me?" For liraglutide, treatment should be discontinued if patients haven't achieved at least 5% weight loss after 12 weeks at the maintenance dose of 3 mg. For semaglutide, assessment typically occurs around 6 months. NHS-funded treatment is usually limited to a maximum of 2 years. Understanding these criteria is important.
Don't hesitate to ask about monitoring requirements: "How often will I need follow-up appointments? What blood tests or health checks will be necessary?" Regular monitoring ensures safety and allows for dose adjustments or early identification of complications.
Finally, discuss long-term planning: "What support will be available for maintaining weight loss? What happens when I stop the injections?" Understanding the comprehensive care pathway, including dietetic support, physical activity guidance, and psychological support, helps you prepare for sustainable success beyond medication alone.
Access to weight loss injections in the UK follows specific pathways depending on whether you pursue NHS or private treatment. NHS eligibility is determined by NICE guidance, which recommends GLP-1 receptor agonists for weight management in adults with a BMI of 35 kg/m² or above (or 32.5 kg/m² for people from South Asian, Chinese, other Asian, Middle Eastern, Black African, or African-Caribbean backgrounds) and at least one weight-related comorbidity, who have not achieved adequate weight loss through lifestyle interventions alone.
Currently, NHS provision of weight loss injections faces significant capacity constraints. Many areas have implemented waiting lists or restricted access to specialist weight management services due to high demand and limited supply. Your GP may refer you to a tier 3 weight management service, where a multidisciplinary team assesses your suitability and provides comprehensive support alongside medication if prescribed. NICE recommends these medications be prescribed within specialist services, typically with a maximum treatment duration of 2 years. Be prepared for potential waiting times of several months.
Private treatment offers faster access but involves substantial ongoing costs. Private prescriptions for semaglutide or liraglutide typically cost between £150–£300 per month (though prices vary and may be affected by supply constraints), representing a significant financial commitment. When considering private options, confirm total costs including medication, consultations, and supplies. Private providers range from online services to specialist weight management clinics. When considering private treatment, ensure the provider is regulated by the Care Quality Commission (CQC) and that prescribers are registered healthcare professionals. For online pharmacies, check they are registered with the General Pharmaceutical Council (GPhC).
Regardless of the pathway, legitimate prescribers will require a thorough medical assessment, including measurement of height, weight, BMI, blood pressure, and often blood tests to check kidney function, liver function, and HbA1c (a diabetes marker). They should discuss contraindications, potential side effects, and the importance of lifestyle modification.
Be cautious of services offering weight loss injections without proper medical assessment or those making unrealistic promises. The MHRA has issued warnings about counterfeit or unlicensed products being sold online. Always verify that you're receiving genuine, licensed medication from a legitimate source. Your safety depends on proper medical oversight throughout treatment.
Setting realistic expectations about weight loss injections is essential for treatment satisfaction and adherence. Clinical trials demonstrate that patients using semaglutide alongside lifestyle interventions lose an average of 10–15% of their body weight over 12–18 months, whilst liraglutide typically results in 5–10% weight loss. However, individual responses vary considerably, and these medications are not effective for everyone. Weight loss occurs gradually, typically 0.5–1 kg per week, and requires patience and persistence.
It's crucial to understand that weight loss injections are not standalone solutions. They work most effectively when combined with reduced calorie intake, increased physical activity, and behavioural changes. Your doctor should emphasise that medication supports—but doesn't replace—lifestyle modification. Many patients find that the appetite suppression provided by these medications makes it easier to adhere to healthier eating patterns.
Discussing potential side effects openly with your doctor helps you prepare for and manage them effectively. The most common adverse effects are gastrointestinal symptoms, including nausea, vomiting, diarrhoea, constipation, and abdominal discomfort. These typically occur when starting treatment or increasing doses and often improve over time. Your doctor may recommend starting with a lower dose and titrating gradually to minimise these effects.
If you have diabetes and take insulin or sulfonylureas, be aware of the increased risk of hypoglycaemia when adding GLP-1 medications. Your diabetes medication doses may need adjustment.
More serious but less common side effects include pancreatitis (inflammation of the pancreas), gallbladder problems, and diabetic retinopathy complications in people with diabetes. Symptoms requiring immediate medical attention include severe abdominal pain, persistent vomiting, or sudden vision changes. Animal studies have shown thyroid C-cell tumours with these medications, though the relevance to humans is uncertain. Report any thyroid symptoms (such as a lump in the neck, hoarseness, or difficulty swallowing) to your doctor.
These medications should not be used during pregnancy or breastfeeding. If you're planning pregnancy, discuss this with your doctor, as semaglutide typically needs to be stopped at least 2 months before conception.
Ask your doctor about strategies for managing side effects, such as eating smaller, more frequent meals, avoiding high-fat foods, staying well-hydrated to prevent dehydration (especially with gastrointestinal side effects), and taking the injection at a time that minimises disruption to your daily routine. Understanding when to contact your GP—such as experiencing severe or persistent symptoms—ensures appropriate safety monitoring throughout your treatment journey.
If you experience any suspected side effects, report them to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk), which helps monitor the safety of medicines.
Bring documentation of your weight history, previous weight loss attempts, a complete list of current medications and supplements, recent blood test results if available, and details of any weight-related health conditions such as type 2 diabetes or hypertension. Prepare written questions and be ready to discuss your lifestyle, eating patterns, and commitment to making concurrent lifestyle changes.
NHS eligibility typically requires a BMI of 35 kg/m² or above (or 32.5 kg/m² for people from South Asian, Chinese, other Asian, Middle Eastern, Black African, or African-Caribbean backgrounds) with at least one weight-related comorbidity, and evidence that lifestyle interventions alone have not achieved adequate weight loss. Treatment is usually provided through specialist weight management services with significant waiting times due to high demand.
The most common side effects are gastrointestinal symptoms including nausea, vomiting, diarrhoea, constipation, and abdominal discomfort, which typically occur when starting treatment or increasing doses and often improve over time. More serious but rare complications include pancreatitis, gallbladder problems, and increased risk of hypoglycaemia in people taking insulin or sulfonylureas for diabetes.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.