Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management, known for its appetite-suppressing effects. Many patients wonder how many calories they should consume whilst taking Ozempic, as the medication significantly reduces hunger and promotes early satiety. There is no single prescribed calorie target—individual needs vary based on age, sex, activity level, and health status. However, maintaining adequate nutrition is essential to preserve muscle mass, support metabolic function, and prevent deficiencies. This article explores evidence-based guidance on calorie intake, balanced nutrition, and safe monitoring whilst taking Ozempic.
Quick Answer: There is no fixed calorie target for Ozempic users, as individual needs vary, but most adults should aim for adequate nutrition—typically 1,400–1,900 calories daily for gradual weight loss—whilst prioritising nutrient-dense foods.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Administered as a once-weekly subcutaneous injection, it works by mimicking the action of naturally occurring GLP-1, a hormone released by the intestine in response to food intake.
The mechanism of action involves several pathways that collectively influence appetite and food consumption. Semaglutide initially slows gastric emptying (though this effect may diminish with continued treatment), meaning food remains in the stomach for longer periods, promoting a sensation of fullness. It also acts on receptors in the hypothalamus—the brain's appetite control centre—to reduce hunger signals and increase satiety. Additionally, Ozempic enhances glucose-dependent insulin secretion and suppresses inappropriate glucagon release, improving glycaemic control in people with type 2 diabetes.
Many patients report a marked reduction in appetite shortly after initiating treatment, often describing feeling satisfied with smaller portion sizes. This effect typically becomes noticeable within the first few weeks of therapy and may intensify as the dose is gradually increased according to the prescribing schedule. Some individuals experience early satiety (feeling full quickly after starting a meal) or a general disinterest in food.
Whilst weight loss is a recognised effect of Ozempic, it is important to note that in the UK, semaglutide is specifically licensed for diabetes management as Ozempic. A higher-dose formulation (Wegovy) is separately licensed for weight management under specific NICE criteria. The appetite-suppressing effects can be substantial, which raises important questions about maintaining adequate nutrition whilst taking this medication.
Patients should be aware that rapid improvements in blood glucose control may be associated with a temporary worsening of diabetic retinopathy in some individuals. It is advisable to report any new or worsening visual symptoms and ensure retinal screening is up to date.
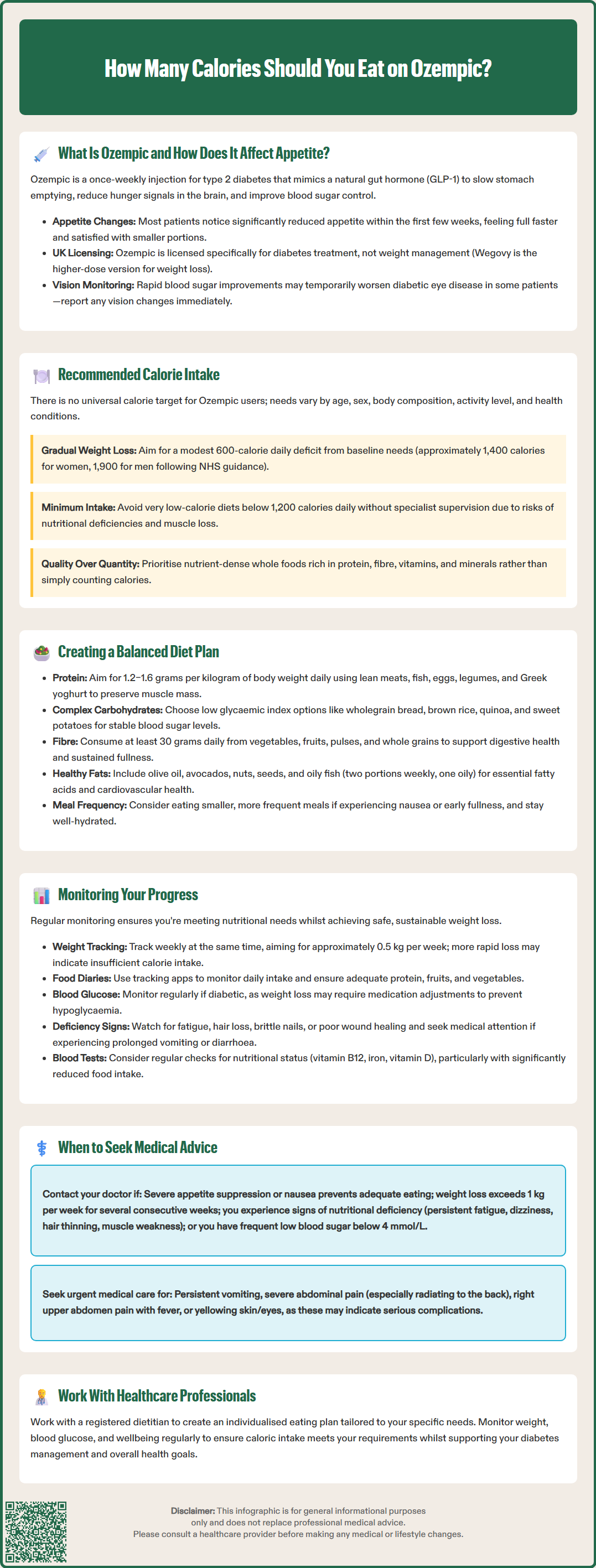
There is no universally prescribed calorie target for individuals taking Ozempic, as nutritional requirements vary considerably based on age, sex, body composition, activity level, and underlying health conditions. However, maintaining adequate caloric intake is essential to support metabolic function, preserve lean muscle mass, and ensure sufficient micronutrient consumption.
For most adults, the NHS recommends a baseline intake of approximately 2,000 calories per day for women and 2,500 for men to maintain weight. When weight loss is desired—whether for metabolic health in diabetes or general weight management—a modest caloric deficit of approximately 600 calories daily typically produces gradual, sustainable weight loss of around 0.5 kg per week. This approach aligns with NHS and NICE guidance on obesity management, which emphasises gradual rather than rapid weight reduction.
It is crucial to focus on nutrient density rather than simply calorie counting. Prioritising whole foods rich in protein, fibre, vitamins, and minerals ensures that even with reduced overall intake, nutritional needs are met. Healthcare professionals may recommend working with a registered dietitian to develop an individualised eating plan that accounts for diabetes management goals, medication effects, and personal preferences. This is particularly important for people with chronic kidney disease, who may need tailored protein recommendations. Regular monitoring of weight, blood glucose levels, and overall wellbeing helps determine whether caloric intake is appropriate for individual circumstances.
Developing a structured, balanced eating plan is essential when taking Ozempic, as the medication's appetite-suppressing effects can inadvertently lead to inadequate nutrition if food choices are not carefully considered. The foundation of a healthy diet whilst on semaglutide should emphasise nutrient-dense foods that provide maximum nutritional value within a potentially reduced caloric intake.
Protein intake deserves particular attention, as adequate protein consumption (approximately 1.2–1.6 g per kilogram of body weight, based on adjusted weight in obesity) helps preserve lean muscle mass during weight loss. Excellent sources include lean poultry, fish, eggs, legumes, Greek yoghurt, and tofu. People with chronic kidney disease should discuss protein targets with their healthcare team. Distributing protein across meals—rather than concentrating it in one sitting—optimises muscle protein synthesis and helps maintain satiety throughout the day.
Complex carbohydrates with a low glycaemic index support stable blood glucose levels, which is particularly important for individuals with type 2 diabetes. Wholegrain bread, brown rice, quinoa, oats, and starchy vegetables like sweet potatoes provide sustained energy and essential B vitamins. Pairing carbohydrates with protein or healthy fats further moderates glucose absorption.
Fibre-rich foods are invaluable, as they promote digestive health, support glycaemic control, and enhance feelings of fullness. The UK recommendation is to aim for about 30g of fibre daily. Vegetables, fruits, pulses, and whole grains should feature prominently in daily meals. Aim for at least five portions of fruits and vegetables daily, as recommended by NHS guidelines.
Healthy fats from sources such as olive oil, avocados, nuts, seeds, and oily fish (salmon, mackerel) provide essential fatty acids and fat-soluble vitamins. The NHS recommends eating two portions of fish weekly, one of which should be oily. Whilst calorie-dense, these foods support cardiovascular health and hormone production.
For those experiencing early satiety or nausea, smaller, more frequent meals may be better tolerated than three large meals, though this is optional—choose an eating pattern that works for you. Staying well-hydrated is equally important, as dehydration can be mistaken for hunger and may exacerbate gastrointestinal side effects sometimes associated with Ozempic. Following the NHS Eatwell Guide proportions can help ensure a balanced approach to nutrition.
Regular monitoring of both nutritional intake and health markers is essential to ensure safe and effective outcomes whilst taking Ozempic. This multifaceted approach helps identify potential issues early and allows for timely adjustments to diet or medication management.
Weight tracking should be conducted consistently—ideally weekly, at the same time of day and under similar conditions (e.g., first thing in the morning, after using the toilet, before eating). Whilst weight is an important metric, it should not be the sole focus. Gradual weight loss of approximately 0.5 kg per week is generally considered safe and sustainable. More rapid weight loss may indicate insufficient caloric intake and warrants discussion with a healthcare provider.
Food diaries or tracking applications can be valuable tools for ensuring adequate nutrition. Recording daily food intake helps identify patterns, such as consistently low protein consumption or inadequate fruit and vegetable intake. These records also provide useful information for healthcare professionals when assessing treatment response and nutritional adequacy.
For individuals with diabetes, regular blood glucose monitoring remains paramount. As weight decreases and insulin sensitivity improves, glucose levels may drop, potentially necessitating adjustments to other diabetes medications to prevent hypoglycaemia. This risk is particularly significant if you are also taking insulin or sulfonylureas—never adjust these medications without consulting your prescriber. HbA1c testing should be conducted according to NICE guidance (typically every 3-6 months) to assess longer-term glycaemic control.
Physical measurements beyond weight—such as waist circumference—offer additional perspective on body composition changes. Muscle mass preservation is important, and some patients may benefit from body composition analysis if available.
Monitoring for adverse effects is equally important. Common gastrointestinal symptoms (nausea, constipation, diarrhoea) may affect food intake and should be reported if persistent or severe. If you experience prolonged vomiting, diarrhoea or signs of dehydration, kidney function should be checked. Signs of nutritional deficiency—such as fatigue, hair loss, brittle nails, or poor wound healing—require prompt medical attention. Regular blood tests to assess nutritional status (including vitamin B12, particularly if also taking metformin, iron, and vitamin D levels) may be appropriate for some patients, particularly those with significantly reduced food intake.
It's also important to report any new or worsening visual symptoms, as rapid improvements in blood glucose can occasionally affect diabetic retinopathy. Ensure you attend regular retinal screening as part of your diabetes care.
Whilst Ozempic is generally well-tolerated, certain situations warrant prompt consultation with your GP or diabetes specialist nurse to ensure treatment remains safe and appropriate.
Seek medical advice if you are consistently unable to consume adequate calories due to severe appetite suppression or persistent nausea. If you're regularly consuming far less than your agreed nutritional plan or experiencing symptoms of undernutrition, your healthcare provider may recommend dose adjustment, anti-nausea medication, or referral to a dietitian.
Rapid or excessive weight loss—more than 1 kg per week over several consecutive weeks—should be discussed with your medical team. Whilst weight reduction is often beneficial, excessively rapid loss can indicate insufficient nutrition and may increase the risk of gallstones, a recognised complication of rapid weight loss.
Signs of nutritional deficiency require prompt evaluation. These include persistent fatigue unrelated to blood glucose levels, dizziness, hair thinning, skin changes, muscle weakness, or difficulty concentrating. Blood tests can identify specific deficiencies that may require supplementation.
For patients with diabetes, frequent hypoglycaemic episodes (blood glucose below 4 mmol/L) or consistently low glucose readings suggest that diabetes medications may need adjustment as insulin sensitivity improves with weight loss. This risk is particularly significant if you are also taking insulin or sulfonylureas. Never adjust diabetes medications independently—always consult your prescriber.
Severe or persistent gastrointestinal symptoms—including intractable nausea, repeated vomiting, severe abdominal pain, or signs of pancreatitis (severe upper abdominal pain radiating to the back)—require urgent medical assessment. Also seek urgent care for symptoms of gallbladder disease (pain in the right upper abdomen, fever, or yellowing of the skin/eyes). Whilst mild gastrointestinal effects are common, severe symptoms may necessitate treatment modification.
Pregnancy or planning pregnancy requires immediate discussion. Semaglutide should be discontinued at least 2 months before a planned pregnancy and is not recommended during pregnancy or breastfeeding.
Finally, if you have concerns about disordered eating patterns or find that the appetite suppression is triggering unhealthy relationships with food, speak with your healthcare provider. Support is available through your GP or organisations like BEAT (the UK eating disorders charity). Psychological support may be beneficial alongside medical management to ensure a healthy approach to nutrition and weight management.
If you experience any suspected side effects from Ozempic, report them through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Very low-calorie diets below 1,200 calories daily should only be followed under specialist supervision, as they carry risks of nutritional deficiencies, muscle loss, and metabolic complications. Consult your healthcare provider before significantly restricting calorie intake.
As weight decreases and insulin sensitivity improves, blood glucose levels may drop, potentially requiring adjustments to other diabetes medications, particularly insulin or sulfonylureas. Never adjust medications independently—always consult your prescriber if experiencing frequent hypoglycaemia.
If severe appetite suppression or persistent nausea prevents adequate calorie intake, contact your GP or diabetes specialist nurse. They may recommend dose adjustment, anti-nausea medication, smaller frequent meals, or referral to a dietitian for personalised nutritional support.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.