
Glucagon-like peptide-1 (GLP-1) receptor agonists are injectable or oral medications used to manage type 2 diabetes and obesity in the UK. Understanding how to take GLP-1 liquid—typically referring to the injectable solution in pre-filled pens—is essential for safe and effective treatment. These medicines work by mimicking a natural hormone that regulates blood sugar, slows digestion, and reduces appetite. Proper administration technique, dosage timing, and storage are crucial to maximising therapeutic benefits and minimising side effects. This guide provides clear, step-by-step instructions aligned with UK clinical guidance to help you use your GLP-1 medication correctly.
Quick Answer: GLP-1 liquid refers to injectable solutions in pre-filled pens, administered subcutaneously into the abdomen, thigh, or upper arm, typically once daily or once weekly depending on the specific medication.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes mellitus and, in some formulations, obesity. These medicines mimic the action of the naturally occurring hormone GLP-1, which is released by the intestine in response to food intake. By activating GLP-1 receptors, these medications enhance insulin secretion when blood glucose levels are elevated, suppress glucagon release, slow gastric emptying, and promote satiety.
In the UK, GLP-1 receptor agonists are available as injectable solutions in pre-filled pens (such as semaglutide [Ozempic, Wegovy], dulaglutide [Trulicity], and liraglutide [Victoza, Saxenda]) or as oral tablets (semaglutide [Rybelsus]). There are currently no licensed oral liquid GLP-1 formulations in the UK. The term "GLP-1 liquid" typically refers to the injectable solution contained within pre-filled pens.
GLP-1 receptor agonists are typically initiated when lifestyle modifications and first-line oral antidiabetic agents (such as metformin) have not achieved adequate glycaemic control. NICE guidance (NG28) recommends their use in specific clinical scenarios, often as part of a stepwise approach to diabetes management. For weight management, NICE technology appraisals (TA875 for semaglutide [Wegovy] and TA664 for liraglutide [Saxenda]) provide specific eligibility criteria. These medications have demonstrated benefits in reducing HbA1c, promoting weight loss, and—for some agents—reducing cardiovascular risk. Understanding the correct method of administration is crucial to maximising therapeutic benefit and minimising adverse effects.
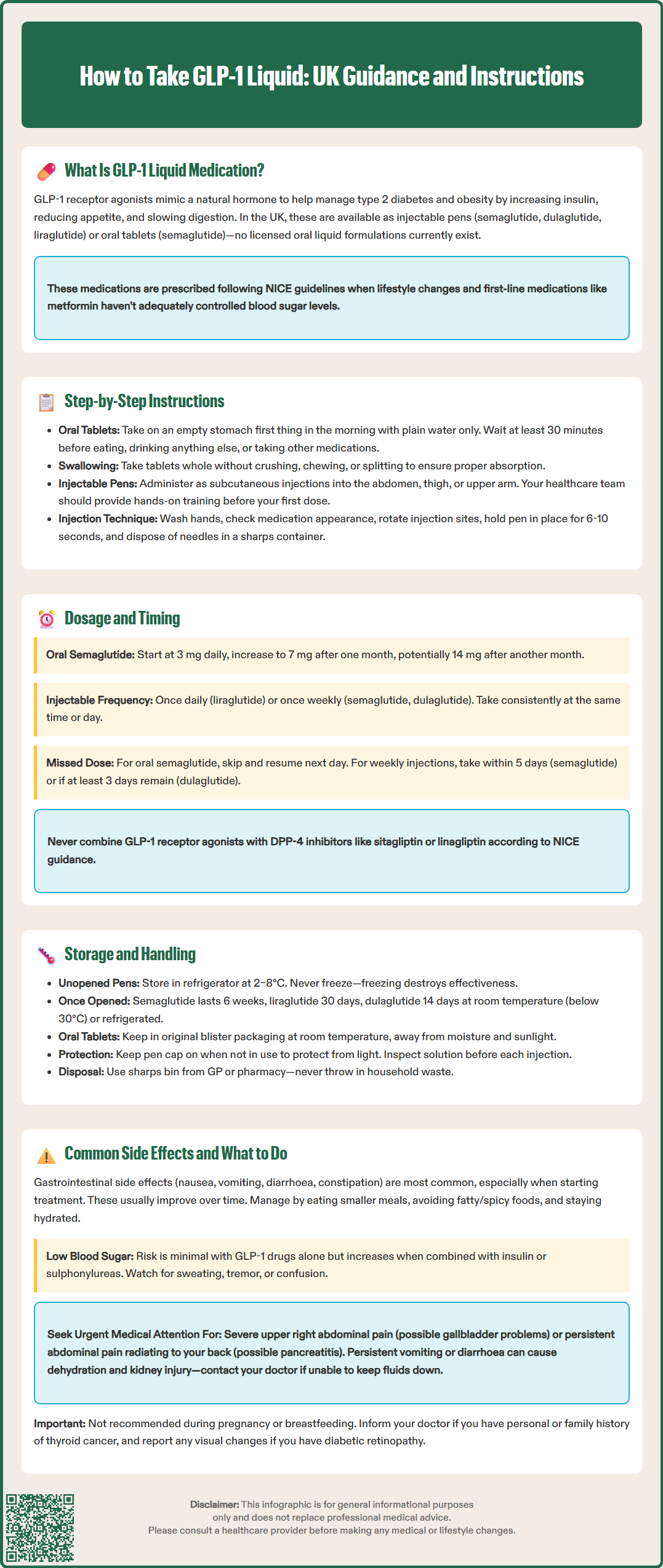
The method of taking GLP-1 medication depends entirely on whether you have been prescribed an oral tablet or an injectable solution. If you have been given an oral GLP-1 medication (such as oral semaglutide [Rybelsus]), follow these steps carefully:
Take the tablet on an empty stomach first thing in the morning, at least 30 minutes before any food, drink (other than plain water), or other oral medications.
Swallow the tablet whole with up to half a glass (approximately 120 mL) of plain water. Do not crush, chew, or split the tablet, as this will reduce absorption.
Wait at least 30 minutes before eating, drinking anything other than water, or taking other medications.
If your prescription is for an injectable GLP-1 solution (contained in a pre-filled pen), the administration route is subcutaneous injection, typically into the abdomen, thigh, or upper arm. Your healthcare team should provide hands-on training before your first dose. Key steps include:
Wash your hands thoroughly and prepare a clean, flat surface.
Check the medication according to the specific product instructions. Most GLP-1 solutions should be clear and colourless to slightly yellow, but some products (like exenatide prolonged-release) are suspensions and appear cloudy by design. Always follow your specific product's Patient Information Leaflet.
Prepare the pen according to manufacturer's instructions. Some pens (like Trulicity) have built-in needles and do not require priming, while others need a new needle attached and priming before each use.
Select an injection site, rotating sites with each dose to prevent lipodystrophy.
Inject subcutaneously at a 90-degree angle, holding the pen in place for the recommended duration (varies by product, typically 6–10 seconds) to ensure full dose delivery.
Always dispose of needles safely in a sharps container. Never share pens or needles with others, and never reuse needles.
Dosage regimens for GLP-1 receptor agonists vary depending on the specific medication, indication (type 2 diabetes or weight management), and individual patient factors. For oral semaglutide (Rybelsus), the typical starting dose is 3 mg once daily for the first month, increasing to 7 mg once daily after 30 days if tolerated. If further glycaemic control is required, the dose may be increased to 14 mg once daily after at least another month. Dose escalation is gradual to minimise gastrointestinal side effects such as nausea and vomiting.
For injectable GLP-1 medications, dosing frequency varies by product. Some are administered once daily (e.g., liraglutide), whilst others are given once weekly (e.g., semaglutide, dulaglutide). Dose escalation schedules are brand-specific—for example, Wegovy (semaglutide for weight management) follows a weekly titration schedule, while Saxenda (liraglutide for weight management) has a daily titration protocol. Your prescriber will provide a clear dosing schedule tailored to your needs. It is important to administer the medication on the same day each week (for weekly formulations) or at the same time each day (for daily formulations) to maintain stable blood levels and optimise efficacy.
Timing considerations are particularly important for oral GLP-1 medications. Taking the tablet at the same time each morning, on an empty stomach, and adhering strictly to the 30-minute waiting period before eating or drinking is essential for adequate absorption. Taking the medication with food can significantly reduce its effectiveness.
If you miss a dose, the guidance depends on the specific product. For once-daily oral semaglutide, skip the missed dose and resume the following day—do not double up. For once-weekly injections, follow your product's specific instructions: for semaglutide injection (Ozempic/Wegovy), administer within 5 days of the missed dose; for dulaglutide (Trulicity), administer if at least 3 days before the next scheduled dose. Always consult your product's Patient Information Leaflet or your prescriber if you are uncertain.
Note that GLP-1 receptor agonists should not be used in combination with DPP-4 inhibitors (e.g., sitagliptin, linagliptin) as per NICE guidance.
Proper storage of GLP-1 medications is essential to maintain their stability, efficacy, and safety. Injectable GLP-1 solutions are biologic medications that require careful handling. Unopened pens should be stored in a refrigerator at 2–8°C and must not be frozen. If a pen has been frozen, it should be discarded, as freezing can denature the active ingredient and render it ineffective.
Once in use, GLP-1 injection pens have product-specific storage requirements:
Semaglutide (Ozempic, Wegovy): Can be stored at room temperature (below 30°C) or in a refrigerator for up to 6 weeks (42 days) after first use.
Liraglutide (Victoza, Saxenda): Can be stored at room temperature (below 30°C) or in a refrigerator for up to 30 days after first use.
Dulaglutide (Trulicity): Single-use pens that may be kept at room temperature (below 30°C) for up to 14 days in total before use.
Always refer to the Patient Information Leaflet specific to your medication for precise storage instructions.
Oral GLP-1 tablets (such as oral semaglutide [Rybelsus]) should be stored in their original blister packaging at room temperature, away from moisture and direct sunlight. Keep the medication in a secure location out of reach of children and pets. Do not transfer tablets to another container, as this may affect stability and increase the risk of medication errors.
Protect injectable pens from light by keeping the pen cap on when not in use. Inspect the solution before each use according to your specific product's instructions—most should be clear and colourless to slightly yellow, but some products are suspensions and appear cloudy by design. Dispose of used pens and needles safely in a sharps bin, which can be obtained from your GP surgery or pharmacy. Never dispose of needles in household waste, as this poses a risk to others. Your local council may offer a sharps disposal service—check with your pharmacist or local authority for guidance.
Gastrointestinal side effects are the most frequently reported adverse reactions with GLP-1 receptor agonists, particularly during the initial weeks of treatment or following dose escalation. These include nausea, vomiting, diarrhoea, constipation, abdominal pain, and reduced appetite. These symptoms are usually mild to moderate and tend to improve over time as your body adjusts to the medication. To minimise discomfort, eat smaller, more frequent meals, avoid high-fat or spicy foods, and stay well hydrated.
If nausea or vomiting is severe or persistent, contact your GP or diabetes specialist nurse. In some cases, temporarily reducing the dose or slowing the rate of dose escalation may be appropriate. Persistent vomiting or diarrhoea can lead to dehydration, which may increase the risk of acute kidney injury, particularly in individuals with pre-existing renal impairment. Seek medical advice if you are unable to keep fluids down or notice a significant reduction in urine output.
Hypoglycaemia (low blood sugar) is uncommon with GLP-1 receptor agonists when used alone, as they work in a glucose-dependent manner. However, the risk increases if you are also taking insulin or a sulfonylurea (such as gliclazide). Symptoms of hypoglycaemia include sweating, tremor, palpitations, confusion, and hunger. If you experience these symptoms, check your blood glucose if possible and treat with fast-acting carbohydrate (e.g., glucose tablets, sugary drink). Discuss with your healthcare team whether adjustment of other diabetes medications is needed.
Gallbladder problems (such as gallstones or inflammation of the gallbladder) have been reported with GLP-1 receptor agonists. Seek urgent medical attention if you develop severe pain in the upper right side of your abdomen, especially if accompanied by fever or yellowing of the skin or eyes.
Patients with pre-existing diabetic retinopathy should be monitored closely, as rapid improvement in blood glucose control may temporarily worsen retinopathy. Report any visual changes to your healthcare provider promptly.
Other potential side effects include injection site reactions (redness, itching, swelling), headache, and fatigue. Rarely, GLP-1 receptor agonists have been associated with pancreatitis (inflammation of the pancreas). Seek urgent medical attention if you develop severe, persistent abdominal pain that radiates to your back, especially if accompanied by nausea and vomiting.
Animal studies have shown thyroid C-cell tumours with some GLP-1 receptor agonists, though the relevance to humans is uncertain. Inform your doctor if you have a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2.
GLP-1 receptor agonists are not recommended during pregnancy or breastfeeding. If you are planning pregnancy, discuss stopping the medication with your healthcare provider in advance.
Report any suspected side effects to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
No, GLP-1 liquid refers to injectable solutions that must be administered subcutaneously. Oral GLP-1 medication (such as oral semaglutide [Rybelsus]) is available as a tablet, not a liquid, and must be taken on an empty stomach with specific timing requirements.
GLP-1 injectable solutions should be administered subcutaneously into the abdomen, thigh, or upper arm. Rotate injection sites with each dose to prevent lipodystrophy and ensure consistent absorption.
For once-weekly injections, administer the missed dose as soon as possible if within the specified timeframe (e.g., within 5 days for semaglutide, at least 3 days before the next dose for dulaglutide). For once-daily formulations, skip the missed dose and resume the following day—never double up. Always consult your product's Patient Information Leaflet for specific guidance.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.