Constipation is a recognised gastrointestinal side effect of Mounjaro (tirzepatide), affecting approximately 6–7% of patients treated for type 2 diabetes mellitus in the UK. Whilst typically mild to moderate, this symptom can impact quality of life and treatment adherence. Understanding why Mounjaro affects bowel function—primarily through delayed gastric emptying and appetite suppression—enables patients to implement effective management strategies. This article explores evidence-based dietary, lifestyle, and hydration approaches to managing constipation on Mounjaro, alongside guidance on when to seek medical advice. Most cases improve with simple interventions, allowing patients to continue benefiting from this dual GLP-1 and GIP receptor agonist.
Quick Answer: Constipation on Mounjaro is managed through increased dietary fibre (30g daily), adequate hydration (1.5–2 litres), regular physical activity, and establishing consistent bowel routines, with medical review if symptoms persist beyond two weeks.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Whilst this medication offers significant benefits in glycaemic control, gastrointestinal side effects are amongst the most commonly reported adverse reactions during treatment.
Constipation is a common side effect of Mounjaro, though it occurs less frequently than nausea or diarrhoea. According to the MHRA-approved Summary of Product Characteristics (SmPC), constipation affects approximately 6–7% of patients receiving tirzepatide, with incidence varying according to dose. The condition is characterised by infrequent bowel movements (typically fewer than three per week), difficulty passing stools, hard or lumpy stools, or a sensation of incomplete evacuation.
For most individuals, constipation associated with Mounjaro is mild to moderate in severity and tends to improve over time as the body adapts to the medication. The symptom typically emerges during the initial weeks of treatment or following dose escalation. Understanding that this is a recognised side effect can help patients manage expectations and implement appropriate strategies early in their treatment journey.
It is important to distinguish between medication-related constipation and other potential causes, such as inadequate fluid intake, reduced physical activity, dietary changes associated with appetite suppression, or concurrent medications (including opioids, iron supplements, anticholinergics, and tricyclic antidepressants). A comprehensive approach to management considers all contributing factors rather than attributing symptoms solely to Mounjaro.
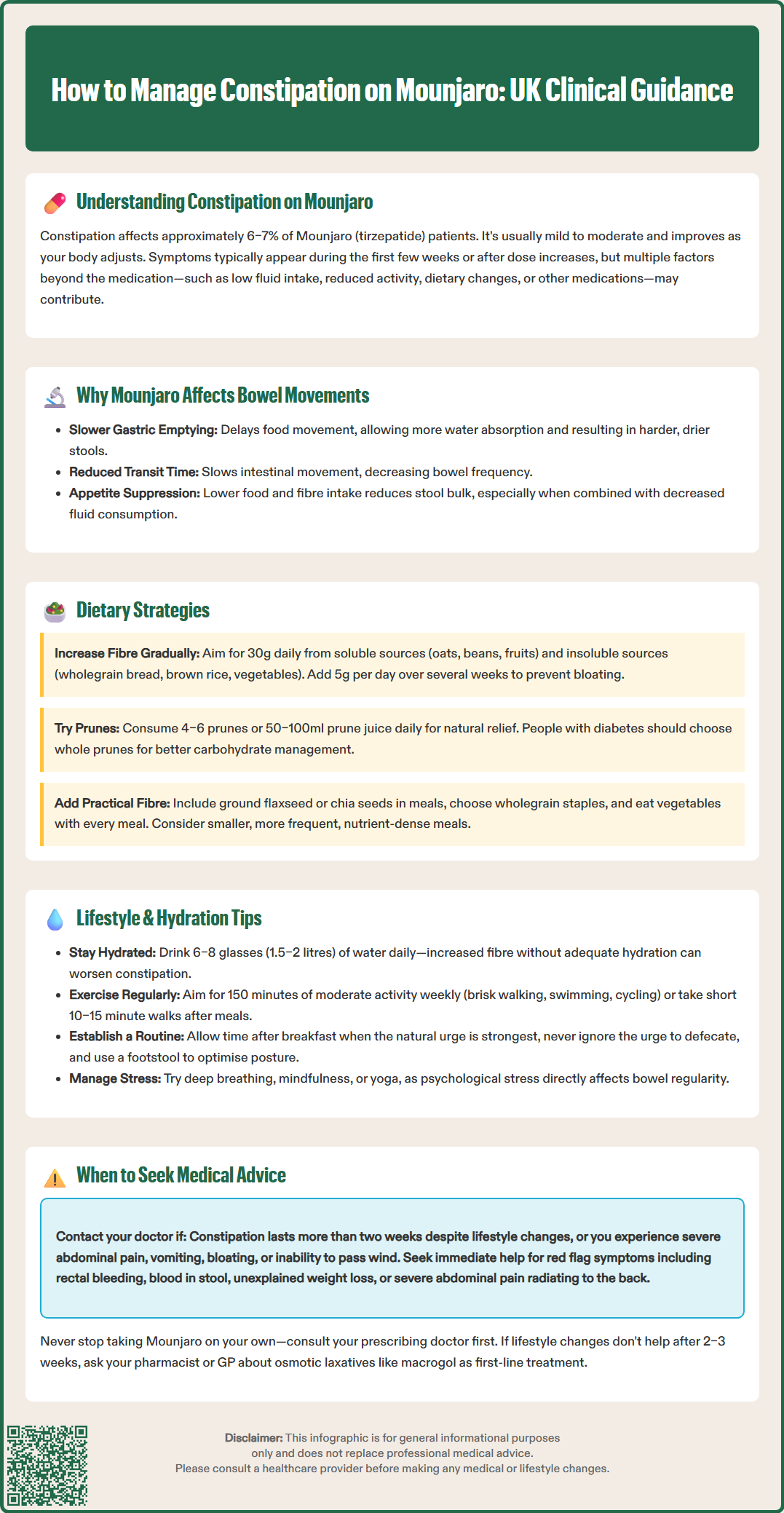
The mechanism by which Mounjaro influences bowel function relates to its pharmacological action on the gastrointestinal tract. As a dual GLP-1 and GIP receptor agonist, tirzepatide primarily slows gastric emptying—the rate at which food moves from the stomach into the small intestine. This delayed gastric emptying contributes to improved glycaemic control and enhanced satiety, and may secondarily affect intestinal transit time.
Delayed gastric emptying is particularly pronounced early in therapy and means that food and waste products move more slowly through the digestive system, allowing more time for water absorption from the stool. This increased water reabsorption results in harder, drier stools that are more difficult to pass. The slowed transit time can also reduce the frequency of bowel movements, contributing to the sensation of constipation. Some adaptation to this effect may occur over time (tachyphylaxis).
Additionally, Mounjaro's effect on appetite suppression may indirectly contribute to constipation. Patients often consume less food overall, which naturally results in reduced stool bulk and frequency. Lower dietary intake, particularly of fibre-rich foods, can compound the constipating effects of the medication itself. Some individuals may also reduce their fluid intake proportionally with decreased food consumption, further exacerbating the problem.
The dose-dependent nature of gastrointestinal side effects means that constipation may become more pronounced as the dose is titrated upwards during treatment. The MHRA-approved dosing schedule for Mounjaro involves gradual dose escalation every four weeks, which allows the body time to adapt. However, each dose increase may temporarily worsen bowel symptoms before tolerance develops. Understanding these mechanisms enables patients and healthcare professionals to implement targeted management strategies that address the underlying causes of medication-related constipation.
Increasing dietary fibre intake represents the cornerstone of managing constipation whilst taking Mounjaro. The Scientific Advisory Committee on Nutrition (SACN) and NHS recommend that adults should aim for 30 grams of fibre daily, incorporating both soluble and insoluble fibre sources. Soluble fibre, found in oats, beans, lentils, and fruits such as apples and pears, absorbs water and forms a gel-like substance that softens stools. Insoluble fibre, present in wholegrain bread, brown rice, nuts, and vegetables, adds bulk to stools and promotes intestinal transit.
Patients should introduce fibre gradually to avoid bloating and excessive gas, which can be particularly uncomfortable when combined with other gastrointestinal effects of Mounjaro. Starting with an additional 5 grams of fibre per day and increasing slowly over several weeks allows the digestive system to adapt. Practical strategies include choosing wholegrain varieties of bread, pasta, and cereals; adding ground flaxseed or chia seeds to yoghurt or smoothies; and ensuring each meal contains at least one portion of vegetables.
Prunes and prune juice may help relieve constipation, as they contain both fibre and sorbitol, a natural laxative compound. Consuming 50–100ml of prune juice or 4–6 prunes daily may help promote bowel movements. However, people with diabetes should be mindful of the carbohydrate content in prune juice and account for this in their dietary management; whole prunes may be preferable. Some studies suggest that kiwi fruit may improve bowel frequency and consistency, and fermented foods such as kefir and sauerkraut may support gut health, though evidence varies.
It is important to maintain adequate nutritional intake despite appetite suppression. Some patients may benefit from smaller, more frequent meals that are nutrient-dense and fibre-rich. Working with a registered dietitian can help ensure that dietary modifications support both diabetes management goals and gastrointestinal health whilst taking Mounjaro.
Adequate hydration is essential for preventing and managing constipation on Mounjaro. The NHS recommends 6–8 glasses (approximately 1.5–2 litres) of fluid daily, with water being the optimal choice. Increased fibre intake without sufficient fluid can paradoxically worsen constipation, as fibre requires water to function effectively. Individuals taking Mounjaro may need to consciously maintain fluid intake even when appetite is reduced. Those with conditions requiring fluid restriction (such as heart failure or kidney disease) should discuss appropriate fluid targets with their healthcare team.
Regular physical activity stimulates intestinal motility and can significantly improve bowel function. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity activity per week, which can be divided into manageable sessions. Activities such as brisk walking, swimming, cycling, or gardening all promote digestive health. Even gentle movement, such as a 10–15 minute walk after meals, can help stimulate bowel activity and reduce the severity of constipation.
Establishing a consistent bowel routine can help train the digestive system. Patients should allow adequate time for bowel movements, particularly after breakfast when the gastrocolic reflex (the urge to defecate following eating) is strongest. Avoiding the urge to delay defecation when it occurs is important, as repeatedly ignoring these signals can worsen constipation over time. Using a footstool to elevate the feet whilst sitting on the toilet can optimise the anorectal angle and facilitate easier passage of stools, as recommended by NHS bowel care resources.
Stress management should not be overlooked, as psychological stress can affect gastrointestinal function. Techniques such as deep breathing exercises, mindfulness, or yoga may help regulate bowel function. Some patients find that keeping a symptom diary helps identify patterns and triggers, enabling more targeted management strategies. If lifestyle modifications prove insufficient after 2–3 weeks, discussing the use of over-the-counter laxatives with a pharmacist or GP may be appropriate. According to NICE Clinical Knowledge Summaries, osmotic laxatives like macrogol are generally preferred as first-line options for medication-related constipation, with bulk-forming laxatives such as ispaghula husk as an alternative (though these should be avoided if obstruction is suspected or in cases of severe abdominal pain or bloating). Patients should report suspected adverse reactions to Mounjaro via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Whilst mild constipation is a recognised side effect of Mounjaro, certain symptoms warrant prompt medical evaluation. Patients should contact their GP or diabetes specialist nurse if constipation persists for more than two weeks despite implementing dietary and lifestyle modifications, or if symptoms significantly impact quality of life. Severe abdominal pain, particularly if accompanied by vomiting, abdominal distension, or inability to pass wind, may indicate bowel obstruction and requires urgent medical assessment via NHS 111, same-day GP appointment, or A&E attendance if severe.
Red flag symptoms that necessitate prompt medical attention include rectal bleeding, blood in the stool (whether bright red or dark/tarry), unexplained weight loss beyond that expected from Mounjaro's therapeutic effect, or a persistent change in bowel habit. In line with NICE guideline NG12, GPs will often arrange a Faecal Immunochemical Test (FIT) and consider urgent referral pathways if indicated. Additionally, severe and persistent abdominal pain, especially if radiating to the back and/or accompanied by vomiting, could indicate pancreatitis—a rare but serious adverse effect associated with GLP-1 receptor agonists that requires immediate medical attention.
If constipation is severe enough to consider discontinuing Mounjaro, this decision should be made in consultation with the prescribing clinician rather than independently. Abruptly stopping the medication may affect glycaemic control, and alternative management strategies may be available. These might include temporary dose reduction, down-titration, or considering alternative treatment options in line with NICE guidance for type 2 diabetes management.
NICE guidance recommends that patients experiencing persistent gastrointestinal side effects from diabetes medications should have their treatment reviewed. Healthcare professionals may need to assess for other contributing factors such as diabetic autonomic neuropathy affecting gut motility, concurrent medications with constipating effects (such as certain analgesics or antidepressants), or underlying conditions like hypothyroidism or hypercalcaemia. A holistic approach ensures that constipation is appropriately managed whilst maintaining optimal diabetes control and overall health outcomes.
Mounjaro (tirzepatide) slows gastric emptying and intestinal transit time, allowing increased water absorption from stools, which results in harder, drier stools that are more difficult to pass. Appetite suppression may also reduce dietary fibre and fluid intake, further contributing to constipation.
Fibre-rich foods such as wholegrain bread, oats, beans, lentils, fruits, and vegetables help promote regular bowel movements. Prunes and prune juice contain both fibre and sorbitol, a natural laxative, and may be particularly effective when consumed daily.
Contact your GP if constipation persists for more than two weeks despite lifestyle modifications, or immediately if you experience red flag symptoms such as rectal bleeding, severe abdominal pain, vomiting, abdominal distension, or inability to pass wind, as these may indicate serious complications.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.