Weight loss injections such as semaglutide (Wegovy) and liraglutide (Saxenda) are GLP-1 receptor agonists licensed in the UK for weight management alongside dietary modification and increased physical activity. Whilst these medications effectively suppress appetite and reduce hunger, choosing the right foods remains essential for nutritional adequacy, managing side effects, and achieving sustainable results. This guide explains what foods to eat on weight loss injections, which foods to limit, and how to create a balanced meal plan that supports both treatment efficacy and long-term health within NHS and NICE guidance frameworks.
Quick Answer: Prioritise lean proteins, non-starchy vegetables, complex carbohydrates, and healthy fats in moderate portions whilst limiting high-fat, fried, and ultra-processed foods to maximise nutrition and manage side effects during GLP-1 treatment.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), work by mimicking naturally occurring hormones that regulate appetite and blood glucose levels. These medications slow gastric emptying, meaning food remains in the stomach longer, which promotes feelings of fullness and reduces hunger signals to the brain. Additionally, they act on areas of the brain involved in appetite regulation, helping to reduce food cravings and overall caloric intake.
Importantly, these medications are licensed in the UK for weight management only alongside a reduced-calorie diet and increased physical activity, generally within specialist weight management services. NICE guidelines (TA875 for semaglutide and TA664 for liraglutide) emphasise that pharmacological interventions should be combined with lifestyle modifications for optimal outcomes. Eligibility is restricted by BMI thresholds and risk factors, meaning not everyone will be suitable for treatment.
Why diet matters during treatment:
Nutritional adequacy – Reduced appetite may lead to insufficient intake of essential nutrients if food choices are poor
Side effect management – Certain foods can exacerbate gastrointestinal symptoms commonly associated with these medications
Metabolic health – Balanced nutrition supports the metabolic improvements these medications facilitate
Long-term success – Developing healthy eating patterns during treatment increases the likelihood of maintaining weight loss after discontinuation
Patients using weight loss injections should view their dietary approach as complementary to the medication, not secondary to it. The reduced appetite provides an opportunity to establish healthier eating habits without the constant battle against hunger that often undermines traditional weight loss efforts.
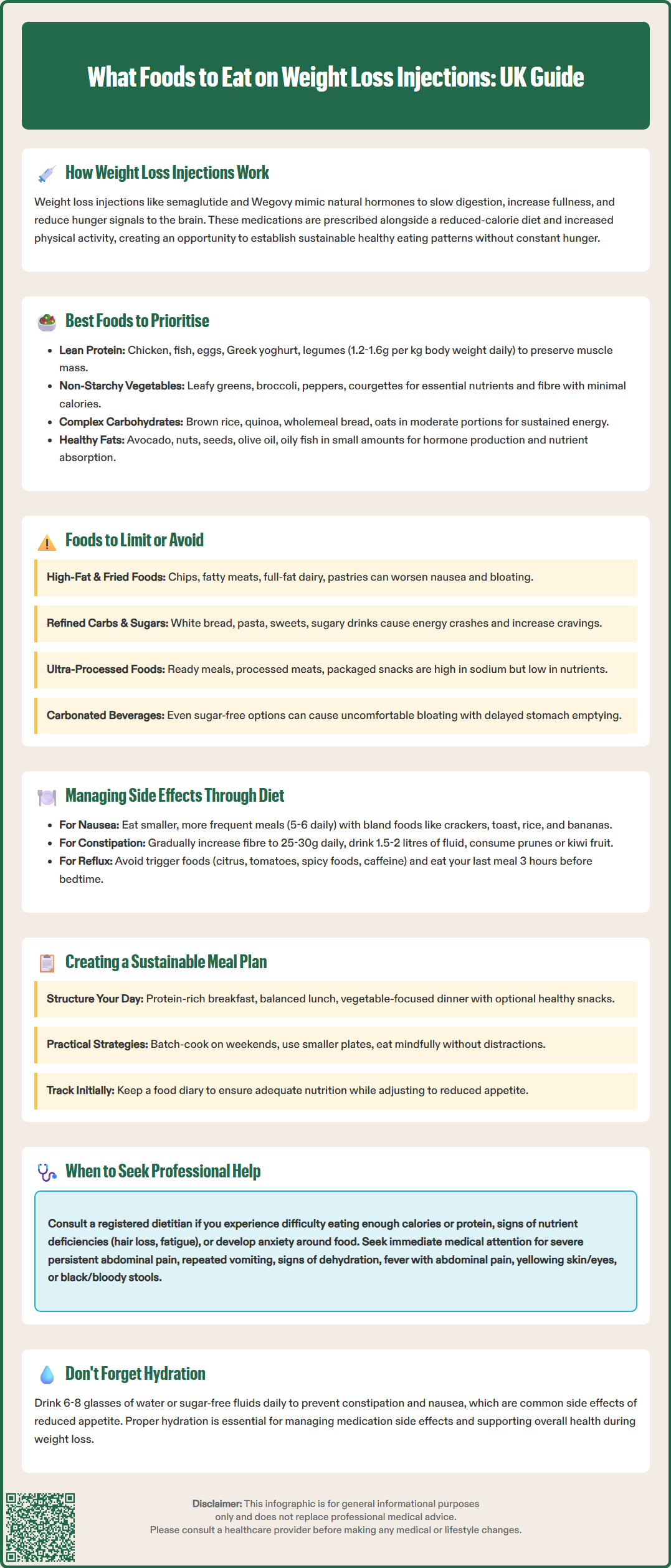
When appetite is suppressed by weight loss injections, every meal becomes an opportunity to maximise nutritional value. Prioritising nutrient-dense foods ensures adequate intake of vitamins, minerals, and macronutrients despite consuming fewer calories overall.
Lean protein sources should form the foundation of your dietary approach. Protein is essential for preserving muscle mass during weight loss, promoting satiety, and supporting metabolic function. Excellent choices include:
Skinless chicken and turkey breast
White fish (cod, haddock, plaice) and oily fish (salmon, mackerel)
Eggs and egg whites
Low-fat Greek yoghurt and cottage cheese
Legumes such as lentils, chickpeas, and beans
Tofu and tempeh for plant-based options
Aim for 1.2–1.6 grams of protein per kilogram of body weight daily to support muscle preservation. If you have a high BMI, this calculation may be based on adjusted body weight rather than actual weight. Those with chronic kidney disease should seek advice from their healthcare provider before increasing protein intake.
Non-starchy vegetables provide essential micronutrients, fibre, and volume with minimal calories. Leafy greens (spinach, kale, rocket), cruciferous vegetables (broccoli, cauliflower, Brussels sprouts), peppers, courgettes, and tomatoes should feature prominently in meals. These foods support digestive health and provide antioxidants that promote overall wellbeing.
Complex carbohydrates in moderate portions help maintain energy levels and provide sustained fuel. Choose wholegrain options such as brown rice, quinoa, wholemeal bread, and oats. These foods have a lower glycaemic index and contain more fibre than refined alternatives, supporting stable blood glucose levels.
Healthy fats in controlled amounts are vital for hormone production, nutrient absorption, and satiety. Include small portions of avocado, nuts, seeds, and olive oil. Oily fish provides omega-3 fatty acids, which have anti-inflammatory properties and support cardiovascular health.
Hydration is equally important. Reduced appetite and gastrointestinal effects may lower fluid intake. Aim for regular fluids (6-8 glasses daily) to help prevent constipation and nausea. Water, herbal teas, and sugar-free beverages are good choices throughout the day.
Certain foods can potentially worsen side effects or provide excessive calories with minimal nutritional benefit. Understanding which foods to limit helps optimise both comfort and results during treatment.
High-fat and fried foods are particularly problematic when using GLP-1 receptor agonists. Because these medications slow gastric emptying, fatty foods may cause or worsen nausea, bloating, and discomfort in many patients. Foods to consider minimising include:
Deep-fried items (chips, battered fish, fried chicken)
Fatty cuts of meat (pork belly, lamb chops with visible fat)
Full-fat dairy products in large quantities
Pastries, cakes, and biscuits high in butter or oil
Creamy sauces and gravies
Refined carbohydrates and added sugars provide rapid energy spikes followed by crashes, potentially increasing cravings and providing calories without nutritional value. Limit white bread, white pasta, sugary cereals, sweets, chocolate, and sugar-sweetened beverages. These foods can also counteract the blood glucose benefits of the medication.
Ultra-processed foods often contain high levels of sodium, unhealthy fats, and additives whilst lacking essential nutrients. Ready meals, processed meats (sausages, bacon, deli meats), and packaged snacks should be occasional choices rather than dietary staples.
Alcohol warrants particular caution. It provides empty calories, can lower inhibitions around food choices, and may worsen gastrointestinal symptoms. For people with diabetes taking insulin or sulfonylureas alongside GLP-1 medications, alcohol may increase hypoglycaemia risk. The UK Chief Medical Officers advise no more than 14 units of alcohol weekly, spread over several days. Many patients find that alcohol tolerance decreases during treatment. If consuming alcohol, do so with food and in moderation.
Carbonated beverages, even sugar-free varieties, may increase feelings of bloating and fullness to an uncomfortable degree when gastric emptying is already slowed. Many patients find still beverages more comfortable during treatment.
Gastrointestinal side effects—particularly nausea, vomiting, constipation, and occasional diarrhoea—are the most commonly reported adverse effects of GLP-1 receptor agonists according to clinical trials and the medicines' Summary of Product Characteristics. Strategic dietary modifications can help reduce the severity and frequency of these symptoms.
For nausea management:
Eat smaller, more frequent meals (5–6 times daily) rather than three large meals
Choose bland, easily digestible foods when nausea is present: plain crackers, toast, rice, bananas
Avoid strong food odours that may trigger nausea
Consume ginger tea or ginger-containing foods, which have natural anti-nausea properties
Eat slowly and chew thoroughly to aid digestion
Avoid lying down immediately after eating; remain upright for at least 30 minutes
For constipation prevention:
Constipation is a common side effect of these medications. Dietary strategies include:
Gradually increasing fibre intake to 25–30 grams daily through vegetables, fruits, wholegrains, and legumes
Ensuring adequate hydration (at least 1.5–2 litres of fluid daily)
Including prunes, kiwi fruit, or linseeds, which have natural laxative properties
Maintaining regular physical activity to stimulate bowel motility
If constipation persists beyond one week despite dietary measures, consult your healthcare provider about appropriate laxatives.
For reflux or heartburn:
Avoid trigger foods such as citrus, tomatoes, spicy foods, and caffeine
Eat your last meal at least three hours before bedtime
Elevate the head of your bed if nighttime symptoms occur
General tolerance tips:
Side effects often improve during or after dose escalation as your body adjusts to the medication. During dose escalation periods, be particularly mindful of portion sizes and food choices.
When to seek urgent medical advice:
Contact your doctor immediately or seek emergency care if you experience:
Severe, persistent abdominal pain (especially if radiating to the back)
Repeated vomiting or inability to keep fluids down
Signs of dehydration (extreme thirst, dry mouth, little or no urination, dizziness)
Fever with abdominal pain or yellowing of the skin/eyes
Black or bloody stools
If you experience any side effects, speak to your doctor, pharmacist or nurse, and report suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Developing a structured yet flexible meal plan helps ensure nutritional adequacy whilst supporting weight loss goals. The objective is to establish eating patterns that can be maintained long-term, extending beyond the treatment period.
Daily structure example:
Breakfast:
Mid-morning snack (if needed):
Lunch:
Afternoon snack (optional):
Dinner (consider eating earlier in the evening):
Practical implementation strategies:
Meal preparation: Batch-cook proteins and grains at the weekend to simplify weekday meals
Portion awareness: Use smaller plates and measure portions initially to recalibrate serving sizes
Mindful eating: Eat without distractions, focusing on hunger and fullness cues
Flexibility: Allow occasional treats in small portions to prevent feelings of deprivation
Monitoring: Keep a food diary initially to identify patterns and ensure adequate nutrition
When to seek professional guidance:
Consult a registered dietitian if you experience:
Difficulty consuming adequate calories or protein
Unintentional nutrient deficiencies (hair loss, fatigue, weakness)
Disordered eating patterns or food anxiety
Uncertainty about appropriate portion sizes
The NHS and specialist weight management services offer dietetic support as part of comprehensive treatment programmes. NICE recommends multidisciplinary care for optimal outcomes (TA875 for semaglutide, TA664 for liraglutide), recognising that successful weight management extends beyond pharmacological intervention alone. By combining the appetite-suppressing effects of weight loss injections with thoughtful, nutritious food choices based on the NHS Eatwell Guide principles, patients can achieve sustainable weight loss whilst supporting overall health and wellbeing.
Whilst weight loss injections reduce appetite, you should focus on nutrient-dense foods rather than eating 'normally'. Prioritise lean proteins, vegetables, and wholegrains in smaller portions to ensure adequate nutrition despite reduced calorie intake, as these medications work best alongside dietary modification.
GLP-1 receptor agonists slow gastric emptying, meaning food stays in the stomach longer. High-fat and fried foods are digested more slowly, which can worsen common side effects such as nausea, bloating, and discomfort during treatment.
Aim for 1.2–1.6 grams of protein per kilogram of body weight daily to preserve muscle mass during weight loss. Choose lean sources such as chicken, fish, eggs, Greek yoghurt, and legumes, and consult your healthcare provider if you have chronic kidney disease before increasing protein intake.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.