
Concerns about whether GLP-1 receptor agonists cause pancreatic cancer emerged from early animal studies and post-marketing reports, prompting regulatory investigations. These medications—including semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), and dulaglutide (Trulicity)—are widely prescribed for type 2 diabetes and weight management in the UK. Understanding the evidence surrounding pancreatic cancer risk is essential for patients and clinicians making informed treatment decisions. Extensive research over the past decade, including large-scale trials and real-world studies, has examined this question thoroughly. Current evidence from regulatory bodies, including the MHRA and EMA, provides reassurance regarding the safety profile of GLP-1 therapies.
Quick Answer: Current evidence does not support a link between GLP-1 receptor agonists and pancreatic cancer.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGLP-1 receptor agonists are a class of medications primarily used to manage type 2 diabetes mellitus and, more recently, obesity. GLP-1 stands for glucagon-like peptide-1, a naturally occurring hormone produced in the intestine that plays a crucial role in glucose regulation and appetite control.
These medications work by mimicking the action of endogenous GLP-1, binding to GLP-1 receptors found throughout the body, particularly in the pancreas, brain, and gastrointestinal tract. The primary mechanisms of action include:
Enhancing insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin is only released when blood glucose levels are elevated
Suppressing glucagon release from pancreatic alpha cells, which reduces hepatic glucose production
Slowing gastric emptying, which helps moderate post-meal blood glucose spikes
Reducing appetite through central nervous system effects, leading to decreased caloric intake and weight loss
Examples of GLP-1 receptor agonists available in the UK include exenatide (Byetta, Bydureon), liraglutide (Victoza for diabetes, Saxenda for weight management), dulaglutide (Trulicity), lixisenatide (Lyxumia), and semaglutide (Ozempic/Rybelsus for diabetes, Wegovy for weight management). These medications are administered either as subcutaneous injections (daily or weekly, depending on the formulation) or, in the case of semaglutide (Rybelsus), as an oral tablet.
The therapeutic benefits of GLP-1 receptor agonists extend beyond glycaemic control. Some agents in this class (liraglutide, semaglutide, and dulaglutide) have demonstrated cardiovascular benefits in patients with established cardiovascular disease, while exenatide showed a neutral effect in cardiovascular outcome trials. The significant weight reduction seen with these medications has made them valuable tools in managing obesity-related complications, as reflected in NICE guidance and technology appraisals for their use in both diabetes (NG28) and weight management.
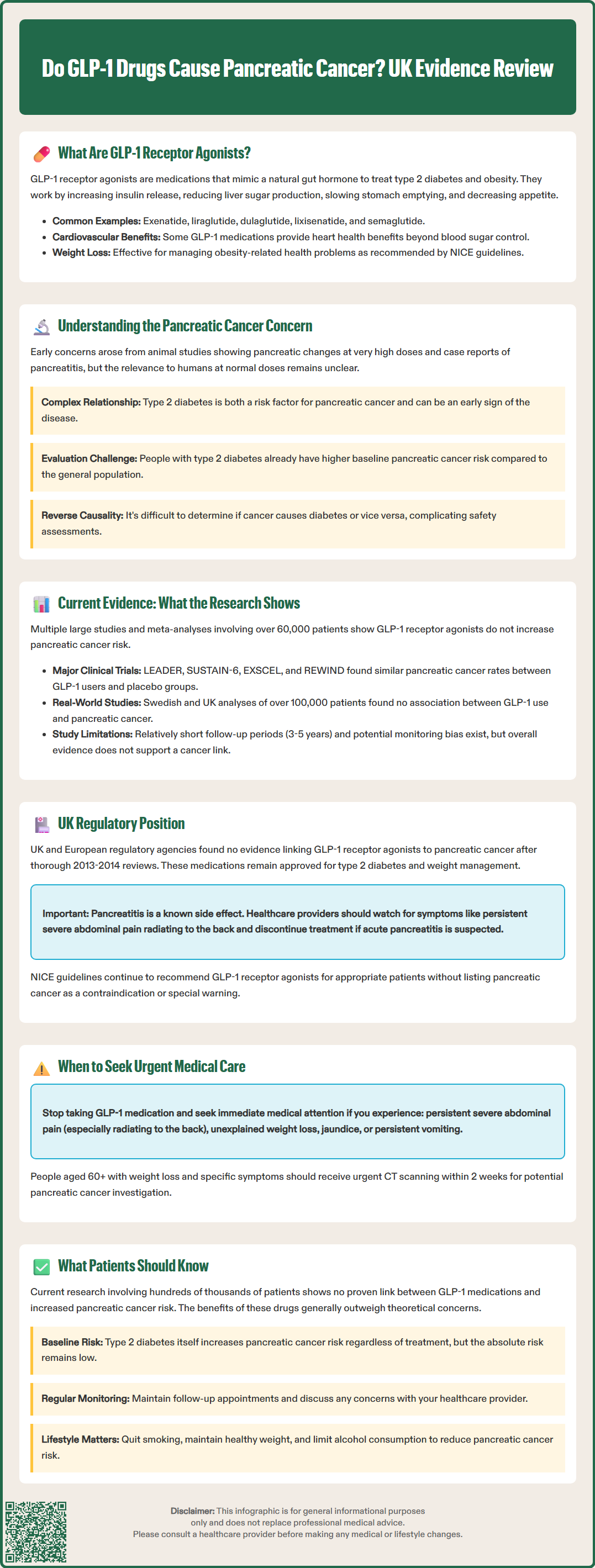
The question of whether GLP-1 receptor agonists might increase pancreatic cancer risk emerged from preclinical animal studies and early post-marketing surveillance reports. These concerns first gained prominence around 2011–2013, when regulatory agencies began investigating potential pancreatic safety signals associated with incretin-based therapies, including both GLP-1 receptor agonists and DPP-4 inhibitors.
Several factors contributed to this concern:
Animal studies in rodents showed pancreatic changes, including increased pancreatic mass and cellular proliferation, when exposed to high doses of GLP-1 analogues over extended periods. However, these findings occurred at exposures significantly higher than therapeutic human doses, and their clinical relevance remains uncertain
Case reports submitted to adverse event databases suggested a possible association between GLP-1 therapy and acute pancreatitis
Theoretical mechanisms were proposed, including chronic pancreatic stimulation and potential effects on pancreatic ductal cells
It is important to understand that pancreatic cancer is relatively rare but carries a poor prognosis, with a five-year survival rate of approximately 5–10%. Risk factors for pancreatic cancer include advancing age, smoking, chronic pancreatitis (not typically acute pancreatitis), family history, obesity, and diabetes itself. This last point is particularly relevant: type 2 diabetes has long been recognised as both a risk factor for and potential early manifestation of pancreatic cancer, creating a complex epidemiological relationship.
The challenge in evaluating GLP-1 safety lies in disentangling drug effects from underlying disease risk. Patients with type 2 diabetes already have an elevated baseline risk of pancreatic cancer compared to the general population. Additionally, pancreatic cancer can itself cause diabetes (reverse causality), making it difficult to determine whether any observed increase in cancer incidence is attributable to the medication or the underlying metabolic condition.
Extensive research over the past decade has provided evidence that GLP-1 receptor agonists do not appear to increase the risk of pancreatic cancer. Multiple large-scale studies, meta-analyses, and cardiovascular outcome trials have specifically examined this question.
A comprehensive meta-analysis published in 2017 examining data from over 60,000 patients found no significant increase in pancreatic cancer risk associated with GLP-1 receptor agonist use. Similarly, major cardiovascular outcome trials—including LEADER (liraglutide), SUSTAIN-6 (semaglutide), EXSCEL (exenatide), and REWIND (dulaglutide)—reported pancreatic cancer incidence rates that were comparable between treatment and placebo groups.
Population-based cohort studies using real-world data have further supported these findings. A large Swedish study published in 2018 analysed over 100,000 patients and found no association between GLP-1 receptor agonist use and pancreatic cancer. Similarly, research using UK primary care databases has not identified an increased risk signal.
Regarding acute pancreatitis—a condition that initially raised concerns—the evidence is mixed, but the absolute risk appears to be low. UK product information (SmPCs) for all GLP-1 receptor agonists includes warnings about pancreatitis. Importantly, if pancreatitis is suspected, the medication should be discontinued immediately, and if acute pancreatitis is confirmed, treatment should not be restarted. The available evidence has not shown that this translates into increased pancreatic cancer incidence in long-term follow-up studies.
Key limitations of current evidence include:
Relatively short follow-up periods (typically 3–5 years) in randomised trials, whereas pancreatic cancer may take years to develop
Potential for detection bias, as patients on GLP-1 therapy may undergo more frequent medical monitoring
Difficulty accounting for all confounding factors in observational studies
Despite these limitations, the weight of current evidence does not support a causal link between GLP-1 receptor agonist use and pancreatic cancer development.
The Medicines and Healthcare products Regulatory Agency (MHRA) and the European Medicines Agency (EMA) have conducted thorough reviews of pancreatic safety data for GLP-1 receptor agonists. Following comprehensive evaluations in 2013–2014, both agencies concluded that available evidence did not support a causal association between these medications and pancreatic cancer.
The current UK regulatory position maintains that:
GLP-1 receptor agonists remain authorised for their approved indications (type 2 diabetes management for all agents; weight management for specific formulations like Saxenda and Wegovy)
Healthcare professionals should remain vigilant for signs of pancreatitis, which is listed as a known adverse effect in the Summary of Product Characteristics (SmPC) for all GLP-1 agents
There is no official link established between GLP-1 therapy and pancreatic cancer based on current evidence
NICE guidance for type 2 diabetes management (NG28) continues to recommend GLP-1 receptor agonists as appropriate treatment options when specific criteria are met. For weight management, NICE has published technology appraisals for specific GLP-1 agents (semaglutide/Wegovy and liraglutide/Saxenda). These guidelines do not include pancreatic cancer risk as a contraindication or special warning.
NICE guidance on suspected cancer recognition and referral (NG12) provides thresholds for urgent investigation of potential pancreatic cancer, including immediate referral for obstructive jaundice, and urgent direct-access CT scanning (within 2 weeks) for people aged 60 and over with weight loss and specific symptoms.
The MHRA's Yellow Card scheme continues to monitor post-marketing safety data, including any reports of pancreatic malignancy. Healthcare professionals and patients are encouraged to report any suspected adverse reactions, contributing to ongoing pharmacovigilance efforts.
Product information for GLP-1 receptor agonists includes guidance on recognising pancreatitis symptoms (persistent severe abdominal pain, often radiating to the back, with or without vomiting) and advises discontinuation if acute pancreatitis is suspected. However, pancreatic cancer is not listed as a specific risk or contraindication in current UK prescribing information.
Regulatory authorities continue to review emerging safety data as longer-term studies become available, ensuring that prescribing guidance reflects the most current evidence base.
Current evidence is reassuring regarding GLP-1 receptor agonists and pancreatic cancer risk. Research to date does not demonstrate an increased risk of pancreatic cancer with these medications. The benefits of improved glycaemic control, weight reduction, and for some agents, cardiovascular protection, generally outweigh theoretical concerns that have not been substantiated by clinical research.
Important points for patients to understand:
No proven link exists between GLP-1 medications and pancreatic cancer based on extensive research involving hundreds of thousands of patients
Type 2 diabetes itself carries an increased risk of pancreatic cancer, independent of treatment
The absolute risk of pancreatic cancer remains low, even in higher-risk populations
Regular medical follow-up allows for monitoring of overall health and early detection of any concerns
When to contact your GP or seek medical attention:
Patients should be aware of symptoms that warrant prompt medical evaluation, including:
Persistent severe abdominal pain, particularly if it radiates to the back (potential sign of pancreatitis) – if this occurs, stop taking your GLP-1 medication and seek urgent medical advice via your GP, NHS 111, or 999 if severe
Unexplained weight loss (not attributable to the expected effects of GLP-1 therapy)
New-onset jaundice (yellowing of skin or eyes) – this requires immediate medical attention
Persistent nausea and vomiting
Unexpected deterioration in diabetes control or new-onset diabetes without typical risk factors
Making informed treatment decisions:
Patients considering or currently taking GLP-1 receptor agonists should:
Discuss any concerns about cancer risk openly with their healthcare provider
Understand their individual risk factors for pancreatic disease
Maintain regular follow-up appointments as recommended
Report any new or concerning symptoms promptly
Continue treatment as prescribed unless advised otherwise by a healthcare professional
Report any suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk)
Lifestyle factors that reduce pancreatic cancer risk—such as smoking cessation, maintaining a healthy weight, and moderating alcohol consumption—remain important regardless of medication use. For most patients, the established benefits of GLP-1 therapy in managing diabetes and obesity far outweigh theoretical concerns about pancreatic cancer that have not been supported by current evidence.
No, extensive research including large trials and real-world studies has not demonstrated an increased risk of pancreatic cancer with GLP-1 receptor agonist use. The MHRA and EMA have reviewed the evidence and concluded there is no established causal link.
Stop taking your GLP-1 medication immediately and seek urgent medical advice, as persistent severe abdominal pain (especially if radiating to the back) may indicate acute pancreatitis. Contact your GP, NHS 111, or call 999 if symptoms are severe.
Yes, type 2 diabetes is recognised as both a risk factor for pancreatic cancer and a potential early manifestation of the disease, independent of any medication use. This makes it challenging to separate drug effects from underlying disease risk in research studies.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.