
Does GLP-1 help with food noise? Many people taking GLP-1 receptor agonists report a significant reduction in persistent, intrusive thoughts about food—a phenomenon often described as 'food noise'. These medications, originally developed for type 2 diabetes and now licensed for weight management, work through brain pathways that regulate appetite and food reward. Clinical evidence and patient experiences suggest GLP-1 treatments may quiet the relentless mental preoccupation with eating, cravings, and meal planning that characterises food noise. This article examines how GLP-1 medications affect food-related thoughts, which treatments are available in the UK, and what to expect from therapy.
Quick Answer: GLP-1 receptor agonists appear to reduce food noise by acting on brain pathways that regulate appetite and food reward, with many patients reporting decreased intrusive food thoughts and cravings.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereFood noise refers to the persistent, intrusive thoughts about food that occupy mental space throughout the day. These thoughts may manifest as constant cravings, preoccupation with the next meal, or difficulty concentrating on tasks due to food-related rumination. It's important to note that 'food noise' is not a formal medical diagnosis in UK clinical guidance, but rather a patient-described concept that has gained recognition as a meaningful description of the cognitive burden some people experience with disordered eating patterns and obesity.
Individuals experiencing food noise often describe a relentless mental commentary about what to eat, when to eat, and how much to consume. This can include:
Frequent thoughts about specific foods, particularly those high in sugar or fat
Difficulty feeling satisfied after meals, leading to continued eating
Planning meals or snacks excessively throughout the day
Emotional distress when food is unavailable or restricted
The impact on eating behaviour can be substantial. Food noise may drive overconsumption beyond physiological hunger, contributing to weight gain and making weight management efforts particularly challenging. Many people report that these intrusive thoughts interfere with work productivity, social interactions, and overall quality of life.
Research suggests that food noise may be linked to dysregulation in appetite-controlling hormones and neural pathways. In individuals with obesity, the brain's reward centres may respond more intensely to food cues, whilst satiety signals may become blunted. This neurobiological basis helps explain why willpower alone often proves insufficient for managing persistent food thoughts.
If you're experiencing significant distress from food-related thoughts or behaviours that feel out of control, it's important to speak with your GP. This is particularly important if you notice signs of disordered eating such as binge eating, severe restriction, purging behaviours, or obsessive thoughts about food. NHS weight management services and eating disorder support are available through GP referral or self-referral in many areas.
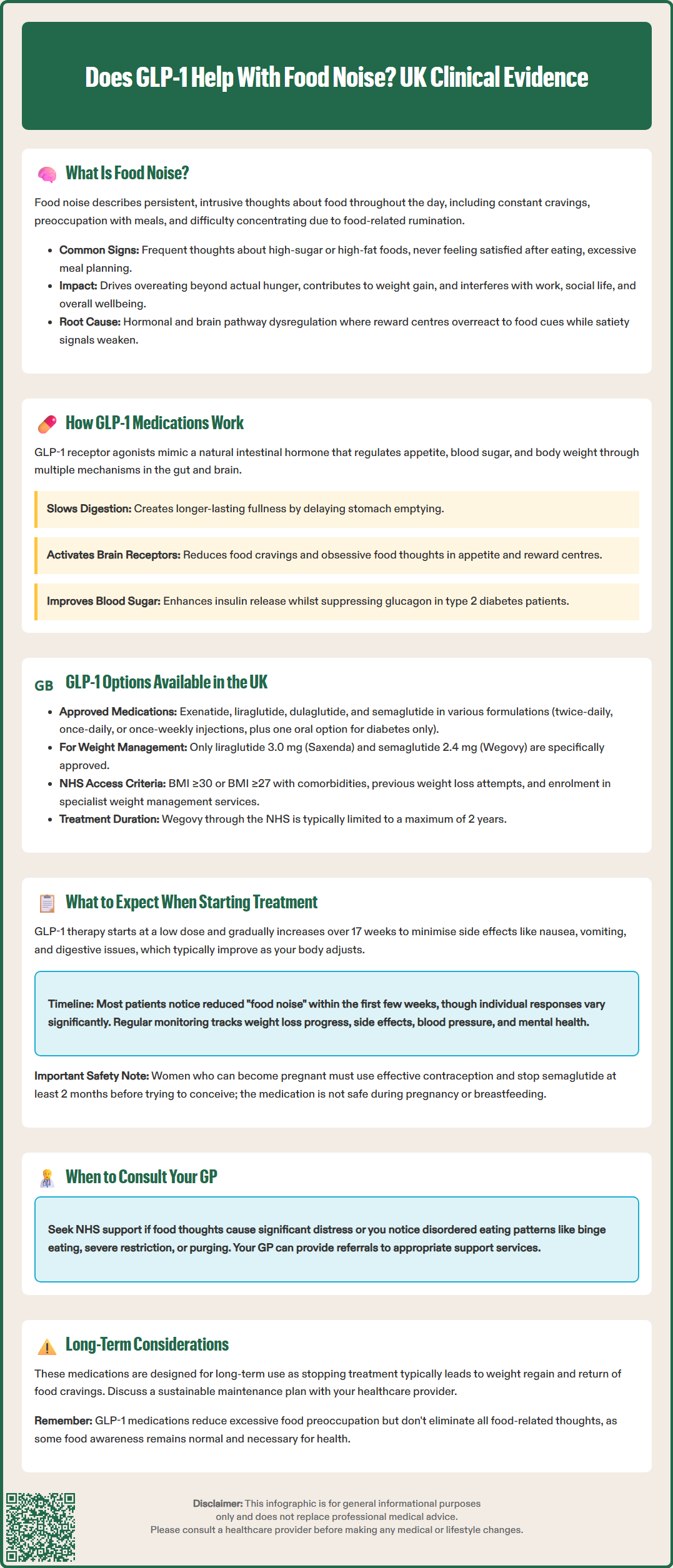
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications that mimic the action of naturally occurring GLP-1, a hormone produced in the intestines in response to food intake. These medications work through multiple complementary mechanisms to regulate appetite, glucose metabolism, and body weight.
In the gastrointestinal system, GLP-1 receptor agonists slow gastric emptying, meaning food remains in the stomach for longer periods. This prolonged gastric distension contributes to earlier and more sustained feelings of fullness after eating, although this effect may attenuate over time with continued treatment. Additionally, these medications enhance glucose-dependent insulin secretion from pancreatic beta cells whilst suppressing inappropriate glucagon release, thereby improving glycaemic control in individuals with type 2 diabetes.
The potential effects on food noise may occur primarily through central nervous system pathways. GLP-1 receptors are present in key brain regions involved in appetite regulation, including:
The hypothalamus, which governs hunger and satiety signals
The nucleus tractus solitarius in the brainstem, which processes signals from the gut
Reward centres such as the ventral tegmental area and nucleus accumbens
By activating these receptors, GLP-1 medications may reduce the rewarding properties of food and diminish food-related thoughts. Clinical studies and patient reports suggest a notable "quieting" of food noise—describing reduced cravings, less frequent thoughts about eating, and an ability to feel satisfied with smaller portions. This effect appears distinct from simple appetite suppression; rather, it may represent a normalisation of appetite signalling that many individuals with obesity have not experienced for years.
GLP-1 receptor agonists have a low risk of hypoglycaemia when used alone. However, when combined with insulin or sulfonylureas, the risk increases significantly, and dose adjustments of these medications may be necessary.
There is no official link established between GLP-1 medications and complete elimination of all food-related thoughts, as some degree of food awareness remains normal and necessary for health.
Several GLP-1 receptor agonists have received approval from the Medicines and Healthcare products Regulatory Agency (MHRA) for use in the United Kingdom. These medications differ in their specific indications, dosing schedules, and availability.
For type 2 diabetes management, licensed GLP-1 medications include:
Exenatide (Byetta, Bydureon) – available as twice-daily or once-weekly formulations
Liraglutide (Victoza) – administered once daily
Dulaglutide (Trulicity) – given once weekly
Semaglutide (Ozempic) – administered once weekly as an injection
Semaglutide (Rybelsus) – taken orally once daily (for type 2 diabetes only, not licensed for weight management)
For weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with weight-related comorbidities, two medications hold specific licences:
Liraglutide 3.0 mg (Saxenda) – once-daily subcutaneous injection
Semaglutide 2.4 mg (Wegovy) – once-weekly subcutaneous injection
Access to these medications through the NHS is governed by NICE guidance. For weight management, NICE Technology Appraisals (TA664 for liraglutide and TA875 for semaglutide) recommend these medications only as part of specialist weight management services. Eligibility criteria include specific BMI thresholds, presence of comorbidities such as type 2 diabetes or cardiovascular disease, and previous weight loss attempts. Notably, Wegovy treatment through the NHS is usually limited to a maximum of 2 years.
Supply constraints have affected availability of some formulations in the UK, particularly semaglutide for weight management. NHS England and the Department of Health and Social Care have issued guidance prioritising existing patients and those with greatest clinical need.
Most GLP-1 medications require subcutaneous injection, usually in the abdomen, thigh, or upper arm. Pre-filled pen devices have made self-administration straightforward for most patients. Oral semaglutide (Rybelsus) is available for diabetes management but is not currently licensed for weight management in the UK.
Initiating GLP-1 therapy requires careful preparation and realistic expectations. These medications are most effective when integrated into a comprehensive weight management programme that includes dietary modification, increased physical activity, and behavioural support.
Dose escalation follows a gradual schedule to minimise gastrointestinal side effects. For semaglutide 2.4 mg (Wegovy), treatment typically begins at 0.25 mg weekly, increasing every four weeks until reaching the maintenance dose of 2.4 mg at week 17. This titration allows the body to adapt to the medication's effects.
Common adverse effects, particularly during dose escalation, include:
Nausea (reported by 20–50% of patients, usually mild to moderate)
Vomiting, diarrhoea, or constipation
Abdominal discomfort or bloating
Reduced appetite (therapeutic effect, but may feel unusual initially)
Fatigue or headache
These effects typically diminish over several weeks as tolerance develops. Eating smaller meals, avoiding high-fat foods, and staying well-hydrated can help manage symptoms. If side effects become severe or persistent, contact your GP or prescribing clinician, as dose adjustment may be necessary. Patients should report any suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Regarding food noise specifically, many patients notice changes within the first few weeks of treatment. The constant mental preoccupation with food often lessens, cravings become less intense, and the ability to stop eating when satisfied improves. However, individual responses vary considerably.
Monitoring and follow-up are essential. Your healthcare team will assess:
Weight loss progress (according to UK product guidance, for Saxenda, treatment should be discontinued if <5% weight loss after 12 weeks at the 3 mg dose; for Wegovy, follow current SmPC guidance on reassessment)
Tolerability and side effects
Blood pressure and metabolic parameters
Psychological wellbeing and eating behaviours
Important safety considerations include:
GLP-1 medications are not recommended during pregnancy or breastfeeding. Women of childbearing potential should use effective contraception during treatment. For semaglutide specifically, it should be discontinued at least 2 months before a planned pregnancy due to its long half-life.
Caution is advised in patients with severe gastrointestinal disease, including gastroparesis.
There is a risk of dehydration and acute kidney injury, particularly if experiencing severe gastrointestinal side effects.
For people with diabetes, there is a potential risk of diabetic retinopathy complications, particularly if there is rapid improvement in glucose control.
When used with insulin or sulfonylureas, dose adjustments of these medications may be needed to reduce hypoglycaemia risk.
Patients should be aware of warning signs of pancreatitis (severe abdominal pain) and gallbladder disease.
A family or personal history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2 requires careful consideration; patients should report any neck mass, hoarseness, or difficulty swallowing.
GLP-1 medications are intended for long-term use; discontinuation often results in weight regain and return of food noise. Discuss treatment duration and maintenance strategies with your healthcare provider to develop a sustainable plan aligned with your individual circumstances and goals.
Many patients notice a reduction in food noise within the first few weeks of GLP-1 treatment, though individual responses vary considerably. The effect typically becomes more pronounced as the dose is gradually increased to the maintenance level.
GLP-1 medications for weight management are available through NHS specialist weight management services following NICE guidance. Eligibility requires specific BMI thresholds (≥30 kg/m² or ≥27 kg/m² with comorbidities) and previous weight loss attempts, not food noise alone.
Discontinuing GLP-1 medication often results in return of food noise alongside weight regain, as the medication's effects on appetite-regulating pathways diminish. Long-term treatment strategies and maintenance plans should be discussed with your healthcare provider.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.