
Does weight loss injections cause hair loss? This question concerns many patients considering or currently using GLP-1 receptor agonists such as semaglutide (Wegovy, Ozempic) and liraglutide (Saxenda) for weight management. Whilst hair loss is not listed as a direct side effect in official prescribing information approved by the MHRA, some patients report increased hair shedding during treatment. Understanding the relationship between these medications and hair health—including the role of rapid weight loss itself—is essential for making informed treatment decisions and managing expectations throughout your weight management journey.
Quick Answer: Weight loss injections such as semaglutide and liraglutide do not directly cause hair loss according to MHRA-approved prescribing information, but temporary hair shedding may occur due to rapid weight loss itself rather than the medication's pharmacological action.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections have become increasingly prominent in the management of obesity and type 2 diabetes in the UK. The most commonly prescribed medications in this category include semaglutide (marketed as Wegovy for weight management and Ozempic for diabetes) and liraglutide (Saxenda). These belong to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists.
These medications work by mimicking a naturally occurring hormone called GLP-1, which is released by the intestines after eating. The mechanism of action involves several physiological processes: they slow gastric emptying (meaning food stays in the stomach longer), reduce appetite by acting on brain centres that control hunger, and improve insulin secretion whilst suppressing glucagon release. This combination leads to reduced calorie intake and subsequent weight loss.
According to NICE guidance (TA875 and TA664), these medications are recommended only within specialist weight management services. Semaglutide (Wegovy) may be considered for adults with at least one weight-related comorbidity and a body mass index (BMI) of 35 kg/m² or above (or 32.5 kg/m² or above for people from South Asian, Chinese, other Asian, Middle Eastern, Black African or African-Caribbean family backgrounds). Liraglutide (Saxenda) has narrower criteria, requiring non-diabetic hyperglycaemia and high cardiovascular risk. Treatment is typically limited to two years.
The medications differ in administration: semaglutide (Wegovy) is given as a weekly subcutaneous injection, while liraglutide (Saxenda) requires daily injections. Weight loss efficacy also varies—semaglutide typically achieves approximately 15% weight loss at 68 weeks, while liraglutide results in about 5-8% weight loss. Doses are gradually increased to minimise gastrointestinal side effects. It's important to note that Ozempic is licensed for type 2 diabetes, not weight management. Understanding the full range of potential effects—including impacts on hair health—remains important for informed treatment decisions.
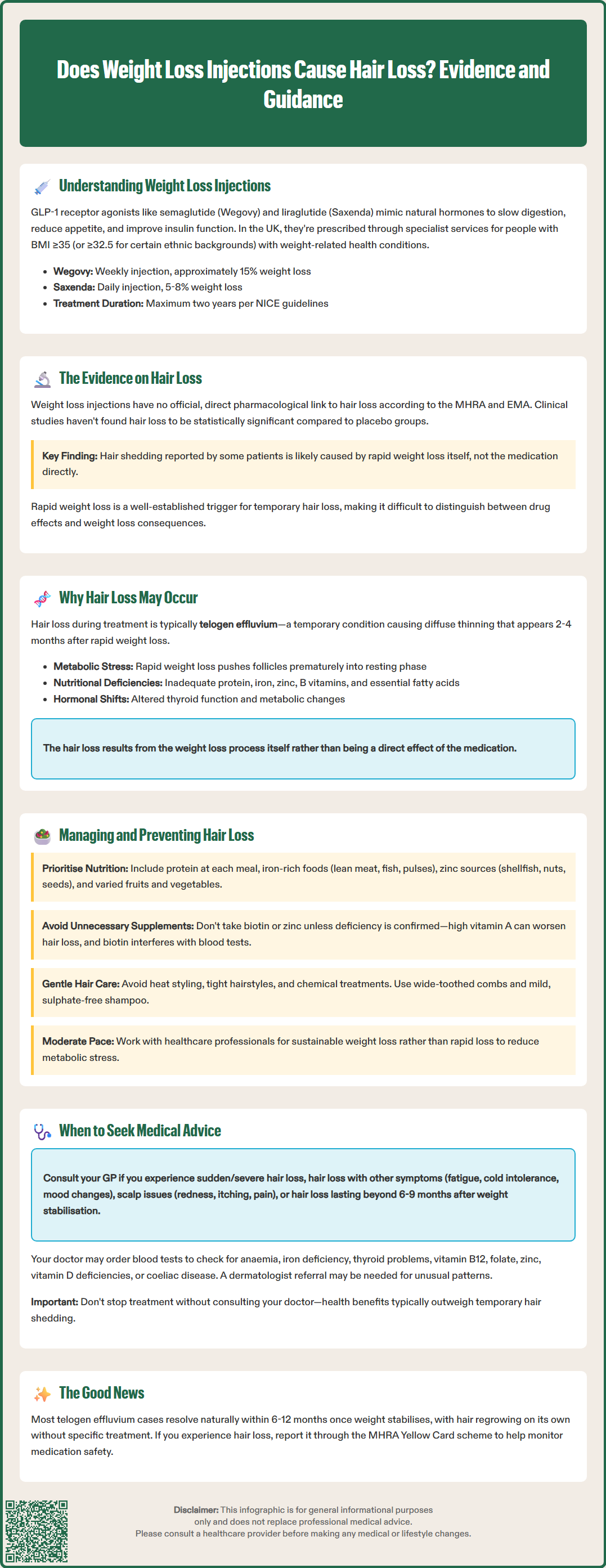
The relationship between weight loss injections and hair loss is complex and not fully established through direct causation. There is no official, direct pharmacological link between GLP-1 receptor agonists and hair loss listed in the Summary of Product Characteristics (SmPC) approved by the MHRA. Hair loss (alopecia) is not documented as a common or recognised adverse effect in the prescribing information for semaglutide or liraglutide.
However, anecdotal reports and patient experiences have raised questions about potential associations. Some individuals using these medications have reported experiencing increased hair shedding, typically several months after starting treatment. It is crucial to distinguish between a direct drug effect and the consequences of rapid weight loss itself, which is a well-established trigger for temporary hair loss.
Clinical studies of GLP-1 receptor agonists have not identified hair loss as a statistically significant adverse event when compared to placebo groups. The European Medicines Agency (EMA) and MHRA continue to monitor post-marketing surveillance data for any emerging safety signals, but hair loss has not been classified as a drug-related adverse reaction requiring specific warnings.
That said, the absence of a documented direct link does not mean patients' experiences should be dismissed. Hair loss during weight loss treatment may occur due to multiple factors related to the weight loss process itself rather than the medication's pharmacological action. Understanding these indirect mechanisms is essential for both patients and healthcare professionals when evaluating symptoms that develop during treatment with weight loss injections.
If you suspect you are experiencing hair loss or any other side effect from your medication, you should report this through the MHRA Yellow Card scheme, which helps authorities monitor medication safety.
When hair loss occurs in individuals using weight loss injections, it is most commonly a condition called telogen effluvium—a temporary form of hair shedding triggered by physiological stress. This condition typically manifests 2-4 months after a triggering event and is characterised by diffuse thinning rather than patchy baldness.
Rapid or substantial weight loss is a well-documented trigger for telogen effluvium. When the body loses weight quickly or undergoes significant calorie restriction, it experiences metabolic stress that can push hair follicles prematurely into the resting (telogen) phase of the hair growth cycle. Subsequently, these hairs shed simultaneously, leading to noticeable thinning. This phenomenon can occur with any method of significant weight loss, whether through medication, surgery, or dietary restriction.
Nutritional deficiencies represent another critical factor. Rapid weight loss and reduced calorie intake may lead to inadequate consumption of nutrients essential for hair health, including:
Protein: Hair is primarily composed of keratin, a protein structure requiring adequate dietary protein for maintenance
Iron: Deficiency is strongly associated with hair loss, particularly in women
Zinc: Plays a vital role in hair tissue growth and repair
Biotin and other B vitamins: Support cellular metabolism in hair follicles (note that high-dose biotin supplements can interfere with certain laboratory tests, including thyroid function and cardiac troponin)
Essential fatty acids: Contribute to scalp health and hair shaft integrity
Additionally, the physiological stress of significant metabolic changes, alterations in hormone levels during weight loss, and potential changes in thyroid function can all contribute to temporary hair shedding. It is worth noting that these factors are consequences of the weight loss process rather than direct effects of the medication itself, though the distinction may feel academic to those experiencing hair loss.
For more information on telogen effluvium, the NHS website and British Association of Dermatologists provide patient resources explaining this condition.
Whilst some degree of hair shedding may be unavoidable during significant weight loss, several evidence-based strategies can help minimise this effect and support hair health throughout treatment.
Optimise nutritional intake by ensuring adequate consumption of key nutrients despite reduced calorie intake. This may involve:
Prioritising protein-rich foods at each meal (protein needs should be individualised; consult a registered dietitian, especially if you have kidney disease or other conditions affecting protein metabolism)
Including iron-rich sources such as lean red meat, poultry, fish, pulses, and dark leafy vegetables
Consuming foods high in zinc (shellfish, meat, seeds, nuts, dairy)
Ensuring adequate vitamin intake through varied fruits and vegetables
Some patients may benefit from a multivitamin supplement, though it is preferable to obtain nutrients from food sources where possible. Avoid taking individual micronutrient supplements (such as zinc or biotin) unless a deficiency has been confirmed by testing or recommended by a healthcare professional. Be aware that some 'hair, skin and nail' supplements may contain high levels of vitamin A, which can paradoxically worsen hair loss. If taking biotin supplements, inform your healthcare provider and consider stopping them 48-72 hours before blood tests, as biotin can interfere with laboratory results, including thyroid and cardiac tests.
Moderate the rate of weight loss where feasible. Whilst GLP-1 medications are effective, working with healthcare professionals to ensure weight loss occurs at a sustainable pace may reduce metabolic stress on hair follicles.
Maintain gentle hair care practices during this period:
Avoid excessive heat styling, tight hairstyles, or chemical treatments
Use a wide-toothed comb and be gentle when hair is wet
Consider a mild, sulphate-free shampoo
Avoid unnecessary hair supplements without professional advice
Address underlying health conditions that may compound hair loss, such as thyroid disorders or iron deficiency anaemia. Regular monitoring through blood tests as recommended by your healthcare provider can identify and address these issues promptly.
Consider discussing your nutrition plan with a dietitian within your specialist weight management service to ensure you're meeting nutritional needs while losing weight.
Whilst telogen effluvium associated with weight loss is typically temporary and self-limiting, certain circumstances warrant medical evaluation to rule out other causes or complications.
Contact your GP if you experience:
Sudden or severe hair loss, particularly if it occurs in patches rather than diffuse thinning
Hair loss accompanied by other symptoms such as fatigue, cold intolerance, unexplained weight changes beyond expected loss, skin changes, or mood alterations (which may suggest thyroid dysfunction)
Scalp symptoms including redness, scaling, itching, or pain (suggesting possible dermatological conditions)
Hair loss persisting beyond 6-9 months after weight stabilisation
Signs of nutritional deficiency such as brittle nails, mouth ulcers, or unusual fatigue
Your GP may arrange blood tests to investigate potential underlying causes, including:
Full blood count (to assess for anaemia)
Ferritin levels (iron stores)
Thyroid function tests (TSH, T4)
Vitamin B12 and folate
Zinc levels (if clinically indicated)
Vitamin D and coeliac serology (if clinically indicated)
In some cases, referral to a dermatologist may be appropriate, particularly if the pattern of hair loss is atypical or if there are concerns about conditions such as alopecia areata or androgenetic alopecia, which require different management approaches.
Discuss the balance of benefits and risks of continuing treatment with your healthcare provider. In most cases, the health benefits of weight loss outweigh the temporary hair shedding, but your clinician may consider dose adjustments or alternative approaches if hair loss is severe or distressing. Do not discontinue treatment without medical consultation.
Most cases of telogen effluvium resolve spontaneously within 6-12 months once the triggering factor stabilises, and hair regrowth occurs naturally. Your healthcare team can provide reassurance, investigate alternative causes, and support you through the treatment journey whilst monitoring both your weight management progress and overall wellbeing.
Hair loss is not listed as a recognised side effect in the MHRA-approved prescribing information for semaglutide (Wegovy) or liraglutide (Saxenda). Any hair shedding experienced during treatment is more likely related to the rapid weight loss process itself rather than a direct drug effect.
Telogen effluvium is the most common type, characterised by temporary, diffuse hair thinning that typically begins 2–4 months after significant weight loss. This condition is triggered by metabolic stress and nutritional changes rather than medication toxicity, and usually resolves within 6–12 months after weight stabilisation.
Ensure adequate protein intake at each meal, consume iron-rich foods and varied nutrients, consider a multivitamin if recommended by your healthcare provider, and maintain gentle hair care practices. Working with a dietitian within your specialist weight management service can help optimise nutrition during treatment.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.