
What is the age limit for weight loss injections in the UK? Weight loss injections such as semaglutide (Wegovy) and liraglutide (Saxenda) have specific age restrictions based on their MHRA-approved licences. Semaglutide is licensed for adults aged 18 years and over, whilst liraglutide can be prescribed to adolescents from 12 years of age who meet specific criteria. For older adults, particularly those aged 75 and above, these medications are used with caution due to limited clinical data. Understanding these age-related guidelines is essential for safe and appropriate prescribing within NHS and private weight management services.
Quick Answer: Weight loss injections have specific age limits: semaglutide (Wegovy) is licensed for adults aged 18 and over, whilst liraglutide (Saxenda) is approved for adults and adolescents aged 12 to under 18 years who meet specific weight criteria.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections represent a relatively recent advancement in obesity management, with medications such as semaglutide (Wegovy) and liraglutide (Saxenda) now licensed in the UK for weight management. These injectable treatments belong to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists, which were originally developed for type 2 diabetes management but have demonstrated significant efficacy in promoting weight loss.
The mechanism of action centres on mimicking the naturally occurring hormone GLP-1, which is released by the intestine after eating. These medications work through several pathways: they slow gastric emptying, which prolongs the feeling of fullness after meals; they act on appetite centres in the brain to reduce hunger signals; and they help regulate blood glucose levels by enhancing insulin secretion when blood sugar rises. This multi-faceted approach typically results in reduced caloric intake, though patients still need to make dietary changes.
Clinical trials have demonstrated different levels of efficacy between these medications. Semaglutide 2.4mg can achieve weight loss of approximately 10-15% of initial body weight over 12-18 months, while liraglutide 3mg typically produces more modest results of about 5-8% weight loss. The injections are administered subcutaneously, usually once weekly (semaglutide) or once daily (liraglutide), using pre-filled pen devices designed for self-administration at home.
It is important to understand that these medications are not cosmetic treatments but prescription-only medicines indicated for chronic weight management in adults with obesity or overweight with weight-related comorbidities. They must be used as part of a comprehensive programme including dietary modification, increased physical activity, and behavioural support. In the NHS, these treatments are typically prescribed within specialist weight management services and, according to NICE technology appraisals (TA875 for semaglutide, TA664 for liraglutide), are generally recommended for a maximum treatment duration of 2 years.
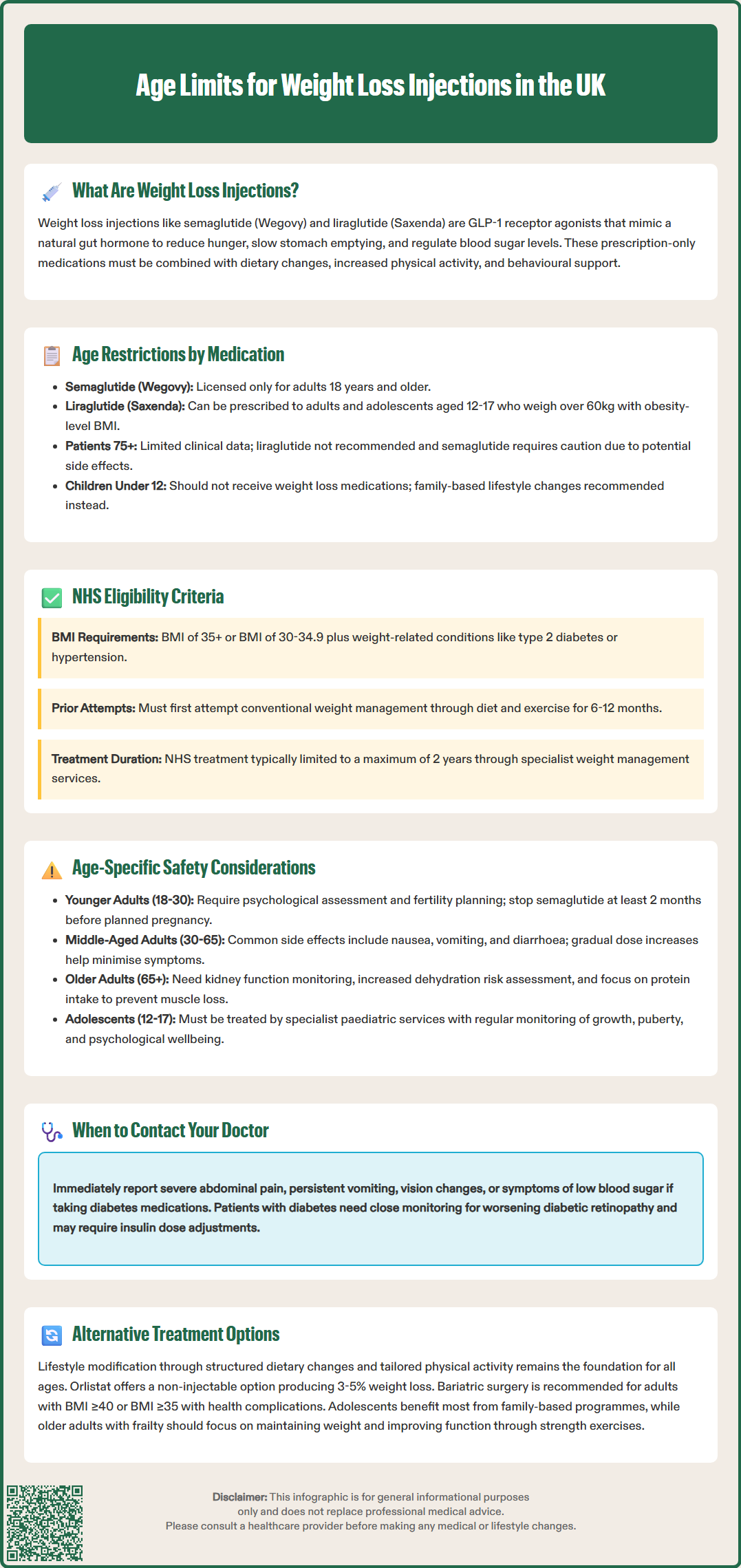
In the United Kingdom, weight loss injections have specific age indications according to their MHRA-approved product licences. Semaglutide (Wegovy) is licensed for use in adults aged 18 years and over only. For liraglutide (Saxenda), the licence includes both adults and adolescents aged 12 to <18 years who weigh more than 60kg and have a BMI corresponding to ≥30 kg/m² for adults.
Regarding upper age limits, while there is no absolute cut-off specified in the product licences, both medications carry important cautions for older adults. The SmPCs (Summary of Product Characteristics) note that there is limited clinical experience in patients aged 75 years and older, and liraglutide is not recommended in this age group. For semaglutide, caution is advised in patients ≥75 years. These cautions reflect the limited inclusion of older adults in clinical trials and potential concerns about side effects in this population.
For adolescents eligible for liraglutide treatment, prescribing should only occur within specialist paediatric services with appropriate expertise in weight management. The medication should be used alongside comprehensive lifestyle interventions tailored to the developmental needs of adolescents. Regular monitoring of growth, pubertal development, psychological wellbeing, and treatment response is essential.
The lower age limit reflects important considerations about growth, development, and the psychological impact of medical weight management interventions during adolescence. For children under 12 years, pharmacological weight management is generally not recommended, with the focus instead on family-based lifestyle interventions.
For older adults, prescribers must consider age-related factors including polypharmacy, renal function, cardiovascular health, and the risk of sarcopenia (muscle loss). The benefits of weight loss must be balanced against potential risks such as falls, frailty, and nutritional deficiencies. Private prescribing practices should align with MHRA-approved indications and professional guidelines, including these age-related considerations.
Eligibility for weight loss injections in the UK follows specific criteria established by NICE technology appraisals (TA875 for semaglutide, TA664 for liraglutide) and general obesity management guidance (CG189). For NHS prescribing, adults are typically eligible for semaglutide if they have a BMI of 35 kg/m² or above, or a BMI of 30-34.9 kg/m² with at least one weight-related comorbidity such as type 2 diabetes, hypertension, dyslipidaemia, obstructive sleep apnoea, or cardiovascular disease. Liraglutide has slightly narrower NHS eligibility criteria, focusing primarily on patients with prediabetes or high risk of cardiovascular disease.
For individuals from Black, Asian, and minority ethnic backgrounds, risk assessment may use lower BMI thresholds (typically 2.5 kg/m² lower) due to the increased risk of type 2 diabetes and other metabolic complications at lower BMI levels in these populations. However, the specific eligibility criteria for medication access follow the NICE technology appraisal recommendations.
Before initiating treatment, patients must demonstrate commitment to lifestyle modification, including dietary changes and increased physical activity. Most services require patients to have attempted conventional weight management approaches for at least 6-12 months without achieving adequate weight loss. A comprehensive assessment should include medical history, current medications, mental health screening, and evaluation of any contraindications.
Contraindications to these medications include: hypersensitivity to the active substance or excipients; pregnancy or breastfeeding; and severe gastrointestinal disease. Caution is required in patients with a history of pancreatitis, gallbladder disease, or diabetic retinopathy. Patients with type 1 diabetes should not use these medications for weight management, as they are not licensed for this indication.
Treatment continuation is based on response. For liraglutide, the SmPC states treatment should be discontinued if patients do not achieve at least 5% weight loss after 12 weeks on the maintenance dose of 3mg daily. For semaglutide, treatment should be discontinued if weight loss of at least 5% has not been achieved after 12 weeks on the maintenance dose of 2.4mg weekly. In the NHS, treatment is typically provided for a maximum of 2 years, within specialist weight management services.
Safety profiles for weight loss injections vary across different age groups, requiring tailored risk assessment and monitoring strategies. For younger adults (18-30 years), the primary considerations include ensuring psychological readiness for long-term treatment, assessing fertility plans, and monitoring for gastrointestinal side effects. For those planning pregnancy, treatment should be discontinued at least 2 months before a planned pregnancy with semaglutide, as specified in the SmPC.
In middle-aged adults (30-65 years), who represent the majority of patients receiving these treatments, safety monitoring focuses on cardiovascular risk factors, glycaemic control in those with diabetes, and the management of common adverse effects. The most frequently reported side effects include nausea, vomiting, diarrhoea, and constipation, which typically improve after the first few weeks. Dose escalation should follow the SmPC-recommended titration schedule to minimise gastrointestinal symptoms. Patients with diabetes should be monitored for potential worsening of diabetic retinopathy, particularly if blood glucose control improves rapidly, and doses of concomitant insulin or sulfonylureas may need adjustment to prevent hypoglycaemia.
For older adults (65+ years), additional safety considerations become paramount. Age-related decline in renal function necessitates baseline and periodic monitoring of kidney function, as dehydration from gastrointestinal side effects poses greater risk. The potential for drug interactions increases with polypharmacy, particularly with medications that affect gastric emptying or require specific timing relative to meals. Older patients face increased risk of sarcopenia, so weight loss should be accompanied by adequate protein intake and resistance exercise to preserve muscle mass. For those aged 75 and over, treatment should be approached with particular caution or avoided (as specified in product SmPCs) due to limited clinical data in this age group.
In adolescents (where licensed for liraglutide), safety monitoring must include growth parameters, pubertal development, bone health, and psychological wellbeing. Treatment should only occur within specialist paediatric services with appropriate multidisciplinary support.
Patient safety advice applicable to all age groups includes: reporting severe or persistent abdominal pain immediately; maintaining adequate hydration; being aware of hypoglycaemia symptoms if taking other glucose-lowering medications; and contacting their GP if they experience persistent vomiting, signs of dehydration, or changes in vision. Patients should be counselled about the importance of continuing treatment only under medical supervision and attending regular monitoring appointments. Any suspected adverse reactions should be reported through the MHRA Yellow Card scheme.
For patients outside the typical age range for weight loss injections, or those who prefer non-injectable options, several evidence-based alternatives exist. Lifestyle modification remains the cornerstone of weight management across all age groups. This includes structured dietary interventions such as calorie-controlled diets, Mediterranean-style eating patterns, or low-carbohydrate approaches, combined with progressive increases in physical activity tailored to individual capability and preferences.
For adolescents and young adults, family-based interventions show particular efficacy. NICE guidance (CG189) recommends multicomponent lifestyle programmes lasting at least 12 weeks, incorporating dietary education, physical activity, and behavioural strategies. Specialist paediatric weight management services provide age-appropriate support addressing the unique psychological and developmental needs of younger patients. Cognitive behavioural therapy (CBT) can help address emotional eating, body image concerns, and motivation for sustainable behaviour change.
Pharmacological alternatives include orlistat, a lipase inhibitor that reduces dietary fat absorption. Prescription orlistat (Xenical 120mg) is licensed for adults and adolescents aged 12 and over with obesity, while over-the-counter orlistat (Alli 60mg) is licensed for adults only. Whilst less effective than GLP-1 receptor agonists (typically producing 3-5% weight loss), orlistat may be appropriate for patients who cannot tolerate injections or have contraindications to GLP-1 medications. The main side effects relate to fat malabsorption, including oily stools and faecal urgency, which can be minimised by adhering to a low-fat diet.
For older adults, particularly those with frailty or multiple comorbidities, the focus may shift from weight loss to weight stabilisation and functional improvement. Supervised exercise programmes emphasising strength and balance can improve mobility and reduce fall risk without necessarily requiring significant weight reduction. Nutritional support should ensure adequate protein and micronutrient intake to prevent malnutrition.
Bariatric surgery represents the most effective intervention for severe obesity across age groups. NICE guidance (CG189) recommends considering surgery for adults with BMI ≥40 kg/m² or BMI ≥35 kg/m² with significant comorbidities who have not achieved adequate weight loss with non-surgical methods. Expedited assessment for bariatric surgery should be considered for people with BMI ≥30 kg/m² who have recent-onset type 2 diabetes. Age alone is not a contraindication, though surgical risk assessment becomes increasingly important in older patients. For adolescents, bariatric surgery may be considered in exceptional circumstances within specialist centres.
Digital health interventions, including the NHS Digital Weight Management Programme, smartphone applications, online support groups, and telehealth consultations, provide accessible alternatives or adjuncts to traditional weight management approaches. These can be particularly valuable for patients in remote areas or those with mobility limitations.
Regardless of the approach chosen, regular monitoring and support from healthcare professionals optimises outcomes. Patients should be encouraged to set realistic goals, celebrate non-scale victories such as improved fitness or better blood pressure control, and understand that weight management is a long-term commitment rather than a short-term fix.
Liraglutide (Saxenda) is licensed for adolescents aged 12 to under 18 years who weigh more than 60kg and have a BMI corresponding to obesity in adults. Prescribing must occur within specialist paediatric weight management services with comprehensive lifestyle support.
Weight loss injections require caution in older adults, particularly those aged 75 and over, due to limited clinical data. Prescribers must carefully assess cardiovascular health, renal function, polypharmacy, and risks such as sarcopenia and frailty before initiating treatment.
Treatment should be discontinued if patients do not achieve at least 5% weight loss after 12 weeks on the maintenance dose. This applies to both semaglutide and liraglutide as specified in their prescribing information.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.