
Glucagon-like peptide-1 (GLP-1) receptor agonists are medications licensed in the UK for managing type 2 diabetes and, in some cases, obesity. Emerging research suggests these drugs may possess anti-inflammatory properties beyond their established metabolic effects. However, no GLP-1 receptor agonist is currently licensed specifically for treating inflammatory conditions, and there is no definitive evidence establishing superiority of one agent over another for anti-inflammatory purposes. This article examines the potential anti-inflammatory mechanisms of GLP-1 medications, compares available agents, and discusses what patients should consider when speaking with their GP about these treatments.
Quick Answer: No single GLP-1 receptor agonist has been proven superior for anti-inflammatory effects, as these medications are not licensed for treating inflammation in the UK.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily licensed in the UK for managing type 2 diabetes mellitus and, in some cases, obesity. These drugs work by mimicking the action of naturally occurring GLP-1, an incretin hormone that stimulates insulin secretion in response to food intake, suppresses glucagon release, and slows gastric emptying. GLP-1 receptor agonists available in the UK include semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and lixisenatide (Lyxumia). Exenatide products have limited availability in the UK.
Beyond their established metabolic effects, emerging research suggests that GLP-1 receptor agonists may possess anti-inflammatory properties. Chronic low-grade inflammation is increasingly recognised as a key contributor to numerous conditions, including cardiovascular disease, metabolic syndrome, non-alcoholic fatty liver disease (NAFLD), and certain autoimmune disorders. The potential anti-inflammatory effects of GLP-1 medications have generated considerable interest among researchers and clinicians.
It is important to emphasise that GLP-1 receptor agonists are not currently licensed specifically for treating inflammatory conditions in the UK. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved these medications for glycaemic control and weight management, not as primary anti-inflammatory agents. Current NICE guidance (NG28 for type 2 diabetes, TA875 for semaglutide 2.4mg, and TA664 for liraglutide 3.0mg) does not include inflammatory conditions as indications.
The UK is currently experiencing supply constraints for some GLP-1 receptor agonists, and NHS England advises against off-label prescribing of diabetes products for weight management alone.
The relationship between GLP-1 receptor agonists and inflammation remains an active area of clinical investigation, with ongoing studies exploring mechanisms and clinical applications beyond traditional metabolic indications.
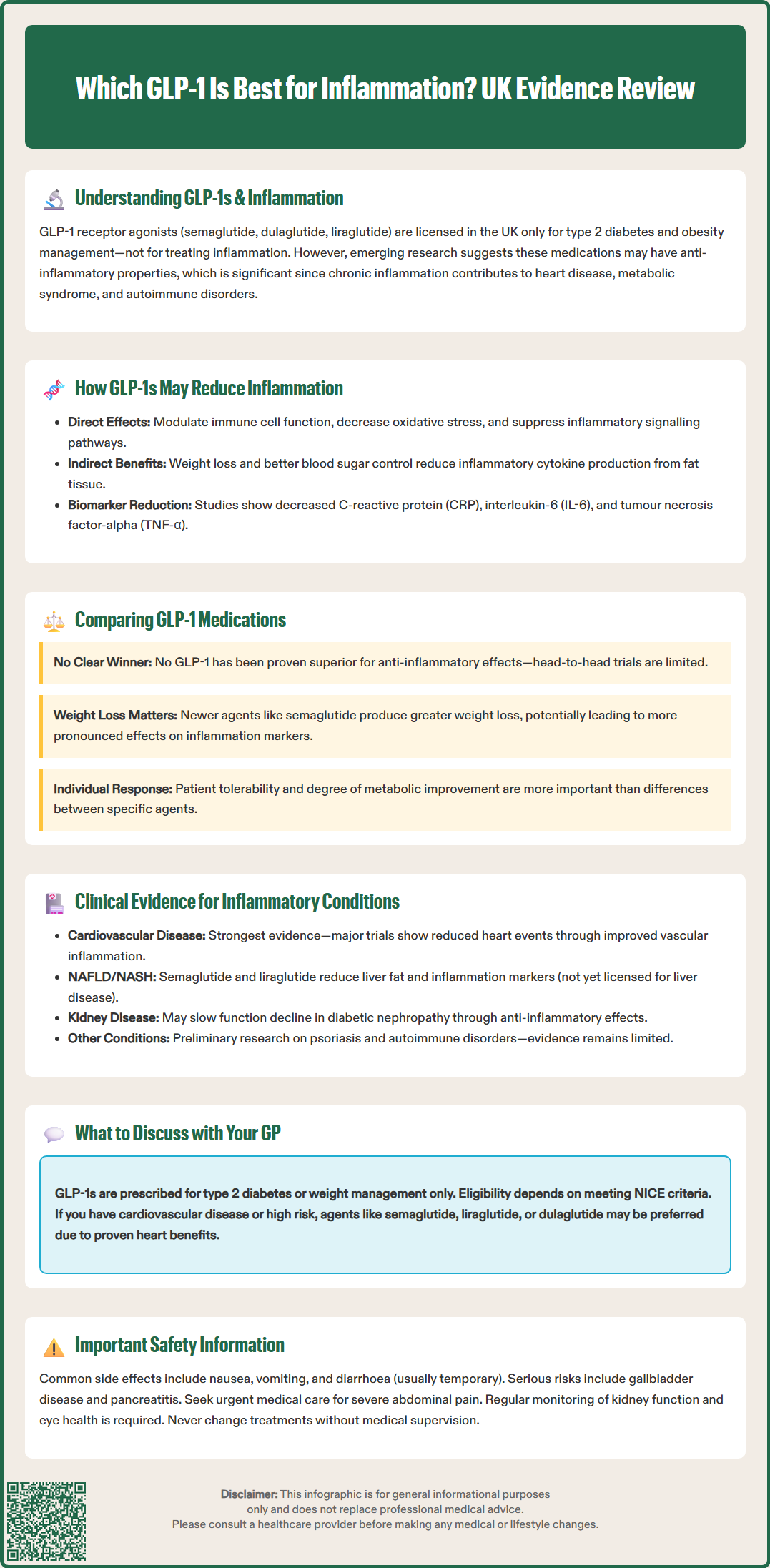
The mechanisms through which GLP-1 receptor agonists may reduce inflammation are multifaceted and not yet fully understood. Research suggests these medications may influence inflammatory pathways both directly and indirectly. GLP-1 receptors are expressed not only in pancreatic beta cells but also in various tissues including the cardiovascular system, kidneys, and immune cells such as macrophages and lymphocytes.
Potential direct anti-inflammatory mechanisms from preclinical and early clinical studies include:
Modulation of immune cell function: GLP-1 receptor activation may reduce pro-inflammatory cytokine production from macrophages and other immune cells
Reduction of oxidative stress: These medications may decrease reactive oxygen species production, which contributes to inflammatory processes
Endothelial protection: GLP-1 receptor agonists may improve endothelial function and reduce vascular inflammation
Inhibition of inflammatory signalling pathways: Including suppression of nuclear factor-kappa B (NF-κB), a key regulator of inflammatory gene expression
It's important to note that many of these mechanisms have been primarily demonstrated in laboratory or animal studies, with more limited evidence in humans.
Indirect anti-inflammatory effects likely result from the metabolic improvements these medications produce. Weight loss, improved glycaemic control, and reduced insulin resistance all contribute to decreased systemic inflammation. Adipose tissue, particularly visceral fat, is metabolically active and produces pro-inflammatory cytokines; reduction in adiposity therefore naturally lowers inflammatory burden.
Clinical studies have demonstrated that GLP-1 receptor agonists can reduce various inflammatory biomarkers, including:
C-reactive protein (CRP): A general marker of systemic inflammation
Interleukin-6 (IL-6): A pro-inflammatory cytokine
Tumour necrosis factor-alpha (TNF-α): Another key inflammatory mediator
Plasminogen activator inhibitor-1 (PAI-1): Associated with cardiovascular inflammation
The magnitude of these effects varies between studies and may depend on baseline inflammatory status, degree of weight loss achieved, and individual patient characteristics. It's important to understand that changes in these biomarkers are surrogate endpoints and have not been validated as a basis for selecting specific GLP-1 receptor agonists for anti-inflammatory purposes.
When considering which GLP-1 receptor agonist might offer the greatest anti-inflammatory benefit, it is crucial to recognise that there is currently no definitive evidence establishing superiority of one agent over another specifically for anti-inflammatory effects. Head-to-head comparative trials examining inflammatory outcomes as primary endpoints are limited, and most evidence comes from individual studies or post-hoc analyses of cardiovascular outcome trials.
Semaglutide, available as once-weekly injection (Ozempic, Wegovy) or daily oral tablet (Rybelsus), has demonstrated robust effects on weight loss and cardiovascular outcomes in the SUSTAIN and STEP trial programmes. Studies suggest semaglutide may reduce CRP and other inflammatory markers, though these effects may be largely attributable to significant weight reduction rather than direct anti-inflammatory action.
Liraglutide (Victoza for diabetes, Saxenda for weight management) is administered as a daily subcutaneous injection. The LEADER cardiovascular outcomes trial demonstrated cardiovascular benefits, and subsequent analyses have shown reductions in inflammatory biomarkers. Some research suggests liraglutide may have effects on immune cell function, though distinguishing these from weight loss effects remains challenging.
Dulaglutide (Trulicity), a once-weekly injection, has also shown cardiovascular benefits in the REWIND trial. Studies indicate improvements in inflammatory markers, though again, distinguishing direct anti-inflammatory effects from those secondary to metabolic improvement remains challenging.
Lixisenatide (Lyxumia) is a daily GLP-1 receptor agonist available in the UK. Its effects on inflammatory markers appear similar to other agents in the class, though with potentially less weight loss benefit than newer agents like semaglutide.
Exenatide products have limited availability in the UK. While they have demonstrated some anti-inflammatory effects in research settings, newer agents generally produce greater weight loss and may therefore have more pronounced effects on inflammation-related markers.
The practical reality is that differences in anti-inflammatory effects between GLP-1 receptor agonists are likely modest and may be overshadowed by individual patient response, tolerability, and the degree of metabolic improvement achieved. NICE guidance (NG28) does not differentiate between agents based on anti-inflammatory properties.
Whilst GLP-1 receptor agonists are not licensed for treating inflammatory diseases, emerging clinical evidence suggests potential benefits in several conditions characterised by chronic inflammation. It is essential to emphasise that these remain investigational applications, and patients should not alter prescribed treatments without medical supervision.
Cardiovascular disease: The most robust evidence for anti-inflammatory benefits comes from cardiovascular outcomes trials. Studies including LEADER (liraglutide), SUSTAIN-6 (semaglutide), and REWIND (dulaglutide) have demonstrated reduced cardiovascular events in patients with type 2 diabetes. Whilst multiple mechanisms likely contribute to these benefits, including improved glycaemic control, weight loss, and blood pressure reduction, changes in vascular inflammation may play a role. Improvements in endothelial function and decreased arterial stiffness have been documented.
Non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH): These conditions involve hepatic inflammation and are closely linked to metabolic syndrome. Clinical trials have shown that GLP-1 receptor agonists, particularly semaglutide and liraglutide, can reduce liver fat content and improve some markers of liver inflammation. The semaglutide NASH trial (NEJM 2021) showed NASH resolution but uncertain effects on fibrosis. Importantly, NICE guidance (NG49) does not currently recommend GLP-1 receptor agonists for the treatment of NAFLD outside clinical trials, and they are not licensed for this indication in the UK.
Chronic kidney disease: Inflammation contributes to progressive kidney damage in diabetic nephropathy. Studies suggest GLP-1 receptor agonists may slow kidney function decline, potentially through anti-inflammatory mechanisms alongside improved glycaemic control and blood pressure reduction. Prescribing should follow current NICE guidance and licensing indications.
Psoriasis and inflammatory skin conditions: Small studies have explored GLP-1 receptor agonists in psoriasis, an inflammatory skin condition often associated with metabolic syndrome. Preliminary evidence suggests potential benefits, though larger trials are needed before any clinical recommendations can be made.
Inflammatory bowel disease and rheumatological conditions: Research in these areas remains very limited, with mostly preclinical or small observational studies. There is currently no official link or recommendation for using GLP-1 receptor agonists as primary treatment for these conditions.
Patients interested in potential anti-inflammatory benefits should discuss the evidence and limitations with their GP or specialist, recognising that these medications are prescribed primarily for metabolic indications according to NICE guidance.
If you are considering a GLP-1 receptor agonist and are interested in potential anti-inflammatory benefits, several important factors should guide the conversation with your GP or diabetes specialist. The choice of medication should be individualised based on your specific medical needs, comorbidities, and treatment goals.
Key discussion points include:
Primary indication: GLP-1 receptor agonists are prescribed for type 2 diabetes management (NICE NG28) or, in specific circumstances, weight management (NICE TA875 for semaglutide 2.4mg; TA664 for liraglutide 3.0mg). Your eligibility depends on meeting NICE criteria, which typically include inadequate glycaemic control despite other medications or specific BMI thresholds for weight management indications.
Cardiovascular risk: If you have established cardiovascular disease or high cardiovascular risk, your clinician may favour agents with proven cardiovascular benefits in outcome trials, such as semaglutide, liraglutide, or dulaglutide.
Weight management goals: If significant weight loss is a priority (which itself reduces inflammation), higher-efficacy agents like semaglutide may be preferred, though individual response varies.
Administration preferences: Consider whether you prefer once-weekly injections (semaglutide, dulaglutide), daily injections (liraglutide, lixisenatide), or oral medication (oral semaglutide), as adherence is crucial for achieving benefits.
Tolerability and side effects: Common adverse effects include nausea, vomiting, diarrhoea, and constipation, which typically improve over time. Other important side effects include gallbladder disease (cholelithiasis, cholecystitis), and potential worsening of diabetic retinopathy (particularly with rapid HbA1c reduction on semaglutide). Rare but serious risks include pancreatitis and, theoretically, thyroid C-cell tumours (based on animal studies). Your GP will assess your individual risk factors.
Important safety considerations:
Seek urgent same-day medical assessment via NHS 111 or A&E for severe abdominal pain (potential pancreatitis) and stop taking the medication pending review
Report persistent nausea, vomiting, or signs of dehydration
Be aware of increased hypoglycaemia risk if taking insulin or sulfonylureas (dose adjustments may be needed)
Attend regular monitoring appointments for kidney function, diabetic retinopathy, and other parameters
Discuss contraception if you are of childbearing potential, as GLP-1 receptor agonists are generally not recommended during pregnancy or breastfeeding
Report any suspected side effects via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk)
Specific administration requirements vary by product. For example, oral semaglutide (Rybelsus) must be taken on an empty stomach with a small amount of water, waiting 30 minutes before eating, drinking, or taking other medications.
Remember that anti-inflammatory effects, whilst potentially beneficial, are not the primary reason for prescribing these medications. The decision should be based on established indications, with any anti-inflammatory benefits considered as potential additional advantages rather than the main treatment goal.
No, GLP-1 receptor agonists are not licensed by the MHRA specifically for treating inflammatory conditions. They are approved for managing type 2 diabetes mellitus and, in certain cases, obesity according to NICE guidance.
GLP-1 receptor agonists may reduce inflammation through direct mechanisms (modulating immune cell function, reducing oxidative stress) and indirect effects from weight loss and improved metabolic control. Clinical studies show reductions in C-reactive protein, interleukin-6, and other inflammatory biomarkers.
There is currently no definitive evidence establishing that one GLP-1 receptor agonist is superior to another specifically for anti-inflammatory effects. Differences between agents like semaglutide, liraglutide, and dulaglutide are likely modest and may be overshadowed by individual patient response and degree of metabolic improvement achieved.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.